Image is for illustrative purposes only.
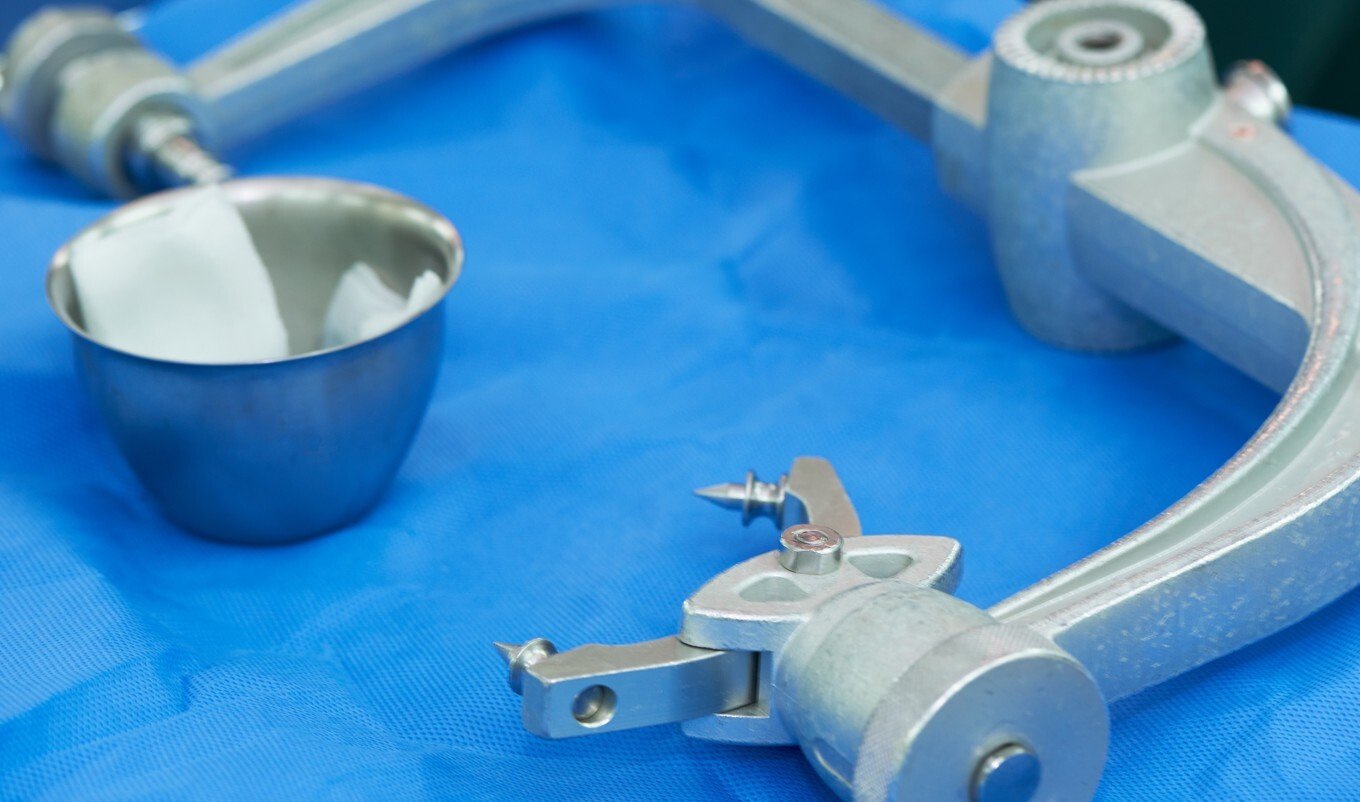
Head Holder, or Similar
GETTING STARTED
This report is a roadmap preview for a Head Holder – not a custom plan. It’s framed as if starting from scratch, highlighting the typical development steps, costs, and hurdles common to devices in this category. Use it to find patterns that apply to your project even if features differ.
As you read:
Look for parallels with your own concept.
Pay attention to phase transitions – that’s where costs and timelines often shift.
Use the benchmarks as reference points, not exact budgets or schedules.
Share it with partners or investors to set realistic expectations from the start.
The aim is to show likely complexities early so you can plan with confidence.
DEVICE OVERVIEW
The proposed medical device is a stationary, large-sized, metal head holder intended for surgical applications. It is a reusable support apparatus designed to stabilize a patient’s head during neurosurgical or cranial procedures, where immobility is critical for safety and precision. Devices in this category are commonly used in operating rooms and neurosurgical suites and may interface with other systems like imaging equipment or surgical navigation tools.
Unlike handheld instruments or portable stabilizers, this device is fixed in position and intended to provide rigid immobilization throughout the procedure. The structural design likely involves complex mechanical parts such as locking joints, adjustable clamps, or articulating arms to allow fine positioning and secure engagement without electronic controls. Given its all-metal construction and lack of electrical components, this head holder relies purely on mechanical engineering for its functionality.
The device is intended for repeated use and is expected to undergo advanced sterilization processes, such as autoclaving, between uses. It comes into direct contact with the patient’s skin, requiring a high degree of biocompatibility and resistance to corrosion or wear under sterilization cycles.
FEASIBILITY
Understanding Your Feasibility Score
The Feasibility Score bar provides an assessment of your project’s path to market, with higher values indicating lower complexity and fewer anticipated obstacles.
- 0 - 39 (Low Feasibility): This range suggests that the project may face significant challenges due to high complexity or extensive requirements. Additional planning, resources, or risk mitigation strategies will be necessary.
- 40 - 74 (Moderate Feasibility): Projects within this range indicate a moderate path to market. While the overall complexity is manageable, some areas may require refinement or further development to ensure project stability and success.
- 75+ (High Feasibility): A score in this range indicates a relatively straightforward path to market, with low complexity and minimal additional work expected. This project is well-positioned to progress smoothly.
The Feasibility Score is a general guide, not an absolute measure of project success. We recommend using this score as part of a broader assessment and considering additional expert guidance for a comprehensive evaluation.
PROJECT OVERVIEW
Note: This report incorporates certain assumptions based on our understanding of typical product development pathways and the stages at which our clients commonly engage with us. Where specific project details were unavailable, we’ve provided informed projections to support strategic planning.
This head holder project is at a very early stage, currently in the concept phase with no previous design iterations, technical documentation, or intellectual property protections in place. While the device concept fits within an established clinical need, particularly in neurosurgery and other head-stabilized procedures, the project is still in the ideation stage with limited formal development progress.
Inventor Stage: Early Exploration
The absence of clinical or institutional support suggests that the inventor is operating independently without a partnered medical team or hospital-based collaborator. This is common at the start of medical device innovation, but securing a clinical champion, such as a neurosurgeon or operating room specialist, will be essential to validate clinical relevance, define user requirements, and guide design decisions.
Device Context: Mechanically Complex but Electrically Simple
Unlike many modern surgical devices that integrate sensors or motorized features, this head holder is non-electronic, which simplifies regulatory and safety requirements but places more design burden on mechanical precision and manual adjustability. Its size and complexity also indicate it will require careful mechanical prototyping and iterative testing to achieve surgical-grade performance and reliability.
What Lies Ahead
To advance, this project will need to move from concept to formal design inputs and verification planning. The inventor should begin by:
- Documenting the use case and performance requirements
- Sketching functional concepts or mockups
- Engaging with clinical end users for feedback
- Defining the basic engineering constraints (e.g., clamping strength, adjustability range, sterilization durability)
Given the lack of existing design assets or development history, the path forward will involve building foundational materials, both technical and strategic, from the ground up.
Strategic Takeaway
This is a mechanically intensive device with no electronics, currently at the idea stage and operating without external validation or documentation. The next steps should prioritize clinical engagement, early concept prototyping, and formalizing design intent, all of which are essential to transitioning from concept to credible development.
COST & TIME ESTIMATES
DEVELOPMENT COMPLEXITY
Understanding what drives or simplifies the development of this head holder is critical to planning resources, timelines, and risk management. As a mechanically complex but electronically simple device, the balance between precision engineering and straightforward design will shape development complexity.
Primary Drivers of Complexity
- Mechanical Precision and Stability
The head holder must maintain rigid immobilization during surgery, often for extended periods. Designing and manufacturing complex mechanical parts like locking mechanisms, clamps, and articulated arms with reliable repeatability demands high precision and quality control. - Material Selection and Durability
Constructed entirely from metal, the device must resist corrosion and degradation from frequent exposure to sterilization processes (e.g., autoclaving). This requires careful selection of biocompatible, sterilization-resistant alloys or coatings. - Surgical Environment Compatibility
The device interfaces directly with patient skin and the sterile field, necessitating materials and finishes that are biocompatible and easily sterilizable without compromising mechanical integrity. - Size and Handling
Its large size and fixed nature introduce challenges in manufacturing, transport, and setup within the operating room, requiring ergonomic considerations and possibly modular design for ease of use.
What Simplifies Development
- No Electronics or Software
The absence of electronic components eliminates complexities related to electrical safety, software validation, and power management. - Simple Supply Chain
The use of mostly off-the-shelf mechanical components can reduce lead times and simplify procurement. - No Customization Required
Designing a standard, non-customized product streamlines development and manufacturing processes.
What Introduces Complexity (and Cost)
- Complex Mechanical Parts
High-precision machining or assembly may increase costs and extend development time. - Advanced Sterilization Requirements
Ensuring materials and assembly methods withstand rigorous sterilization adds testing and validation steps. - Lack of Existing Documentation or IP
Starting without prior designs or patents means that all development and documentation must be created anew, which can be resource-intensive.
Strategic Takeaway
The main complexity of this head holder lies in mechanical engineering and material durability rather than electronics or software. While development benefits from a simple supply chain and no customization, ensuring reliable surgical performance and sterilization compatibility will require focused engineering effort, careful material choices, and thorough testing.
TECHNOLOGICAL READINESS
This section assesses where the head holder stands in its development lifecycle, what technical assets are currently available, and what next steps are needed to progress towards a validated, market-ready product.
Current Stage of Development
The project is in the concept phase, meaning the device currently exists as an idea or perhaps a rudimentary proof-of-concept without physical prototypes or formal designs. No technical documentation or iterations have been completed. This early stage offers flexibility to refine requirements but also requires foundational work to establish a clear development roadmap.
Existing Technical Assets
At this point, there are no existing patents, technical documents, or prototypes. The absence of intellectual property protection indicates an opportunity to establish unique design elements as the project progresses but also means that patent searches and freedom-to-operate analyses will be important early steps.
No clinical or institutional support is yet secured, which means end-user feedback and clinical validation will need to be actively pursued to ensure design relevance and acceptance.
What Comes Next
Key activities to advance technological readiness include:
- Concept Refinement
Develop detailed sketches or computer-aided designs (CAD) to translate the idea into tangible engineering requirements. - Prototyping
Build physical prototypes to test mechanical functionality, adjustability, and fixation strength. - Documentation
Create technical files, including design history, materials specifications, and intended use descriptions. - Preliminary Risk Analysis
Identify potential safety and performance risks early, particularly related to mechanical stability and sterilization compatibility. - Engage Clinical Partners
Collaborate with surgeons or operating room personnel to validate clinical needs and usability. - Plan Verification and Validation
Develop a testing strategy to confirm mechanical performance and sterilization resilience.
Strategic Takeaway
The head holder is at a foundational stage with no physical or documented assets yet developed. Advancing will require structured progression from concept definition through prototyping and documentation, underpinned by clinical input and early risk assessment to guide a smooth transition into later-stage development.
REGULATORY APPROVAL
Understanding the regulatory pathway is essential to plan the device development in compliance with FDA requirements and to anticipate potential hurdles.
Risk Classification and Submission Type
The head holder is classified as a Class II medical device, which means it poses a moderate risk to patient safety and requires regulatory controls beyond general controls. For most Class II devices, including head holders, the typical FDA submission pathway is a 510(k) premarket notification. This pathway requires demonstrating that the device is substantially equivalent to a legally marketed predicate device.
Class II designation reflects the device’s intended surgical use and direct patient contact, necessitating evidence of mechanical safety, biocompatibility, and sterilization compatibility.
FDA Classification Snapshot
- Regulation Number: 882.4460
- Product Code: HBL
- Regulation Medical Specialty: Neurology
- Device Class: Class II
- Submission Pathway: 510(k) Premarket Notification
You should work with a regulatory consultant to verify the correct classification and any associated guidance documents.
Key Regulatory Considerations
- Predicate Comparison
To succeed in the 510(k) pathway, the head holder must be compared to an existing legally marketed device with similar intended use and technological characteristics. Careful selection of an appropriate predicate device and demonstration of equivalence in performance and safety are crucial. - Biocompatibility Testing
Since the device contacts patient skin, it must meet ISO 10993 biocompatibility standards, particularly for cytotoxicity and irritation. - Sterilization Validation
The device is reusable and will undergo advanced sterilization. Validation of sterilization processes, such as autoclave compatibility, must be conducted and documented according to FDA and ISO standards. - Mechanical Performance Testing
Verification and validation testing should demonstrate that the head holder reliably immobilizes the patient’s head without risk of slippage or failure during surgery. - Labeling Requirements
The device labeling must provide clear instructions for use, including sterilization procedures, contraindications, and warnings.
International Considerations
If international markets are targeted, the device will likely be subject to similar regulatory requirements emphasizing mechanical safety, biocompatibility, and sterilization. Harmonizing documentation to meet international standards (e.g., CE marking in Europe) may be advantageous.
Strategic Takeaway
The regulatory path for this head holder centers on the 510(k) process, relying on demonstration of substantial equivalence to an existing device. Attention to biocompatibility, sterilization validation, and robust mechanical testing will be key pillars of a successful submission, with labeling and clinical usability supporting overall compliance.
MARKET POTENTIAL
Evaluating market potential helps align development efforts with commercial realities, ensuring the device meets both clinical needs and business goals.
Market Drivers
The primary drivers for this head holder include:
- Growing demand for neurosurgical and cranial procedures worldwide, driven by aging populations and advances in surgical techniques.
- Need for reliable immobilization to improve surgical precision, patient safety, and outcomes.
- Increasing emphasis on sterilizable, reusable surgical equipment to reduce hospital costs and environmental impact.
Target Segments
The head holder will primarily serve:
- Hospitals and surgical centers with neurosurgery or cranial surgery programs.
- Specialty clinics focusing on neurological or craniofacial procedures.
- Potentially, research institutions conducting experimental surgical techniques requiring stable head fixation.
Adoption Enablers
- Proven mechanical reliability and ease of use will encourage adoption by surgeons and operating room staff.
- Compatibility with standard sterilization protocols supports integration into existing hospital workflows.
- Competitive pricing compared to established devices, especially if manufactured with cost-effective materials and supply chains.
Revenue Considerations
- The device’s reusable nature means revenue relies on initial sales volume and potential aftermarket services (e.g., maintenance, replacement parts).
- Strong regulatory clearance and clinical validation will enable easier market entry and customer trust.
- Opportunity exists to explore leasing models or bundled sales with surgical equipment providers.
Revenue Risk Factors
- The presence of established competitors with strong brand recognition.
- Limited differentiation in device functionality may reduce pricing power.
- Dependence on hospital capital budgets, which can fluctuate due to economic factors.
Strategic Takeaway
While the head holder addresses a well-defined surgical need in a growing market, its non-unique design and competitive landscape emphasize the importance of delivering proven mechanical reliability and cost-effectiveness. Early clinical validation and clear value communication will be critical to capturing market share.
DEVELOPMENT PHASES & MILESTONES
A structured development plan helps ensure steady progress from concept to market-ready device. Below is a recommended phased approach tailored to the head holder’s early-stage status and mechanical complexity.
Phase I: Concept Development
Goal: Define the device’s intended use, design requirements, and preliminary functionality.
Key Activities:
- Document surgical requirements and user needs
- Sketch initial design concepts
- Perform early risk identification
Milestone: Approved concept design and development plan ready for prototyping.
Phase II: Prototype Development
Goal: Build and test physical prototypes to evaluate mechanical performance and ergonomics.
Key Activities:
- Create CAD models and engineering drawings
- Manufacture prototypes using suitable materials
- Conduct functional tests (stability, adjustability)
- Engage clinical advisors for feedback
Milestone: Working prototype validated for next-stage design refinement
Note: The regulatory cost estimates in this section include expenses associated with an optional FDA 510(k) pre-submission (Q-Sub), which, while not required, can be a valuable tool for obtaining early feedback and reducing downstream submission risk.
Phase III: Design Output & Verification
Goal: Finalize detailed design and verify performance against requirements.
Key Activities:
- Produce detailed design documentation and specifications
- Conduct verification testing per defined protocols (mechanical strength, sterilization resistance)
- Refine design based on test results
Performance Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Static Load Testing | Internal protocol | Ensures the device can withstand expected surgical forces |
| Slip/Displacement Testing | Internal protocol | Verifies head remains immobilized under stress/load |
| Adjustment Mechanism Reliability | Internal protocol | Validates long-term use of mechanical parts |
| Durability Under Reuse | Simulated use cycles + sterilization cycles | Confirms mechanical integrity over repeated cleaning/use |
Biological Safety Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Cytotoxicity | ISO 10993-5 | Ensures materials in contact with skin do not cause cell damage |
| Irritation | ISO 10993-10 | Evaluates skin irritation potential |
| Sensitization | ISO 10993-10 | Assesses potential to cause allergic response |
Phase IV: Validation & Regulatory Submission
Goal: Validate device performance in simulated or clinical settings and prepare regulatory submission.
Key Activities:
- Perform validation testing (sterilization, biocompatibility, usability)
- Compile technical file and 510(k) submission documents
- Address any regulatory queries or requests
Milestone: Regulatory clearance obtained.
Packaging and Environmental Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Sterility Maintenance | ISO 11607 | Ensures packaging maintains sterility until point of use |
| Transportation Simulation | ASTM D4169 | Verifies package integrity through shipping and handling |
Usability Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Human Factors Evaluation | IEC 62366-1 | Validates ease of use and risk controls for clinical users |
| Cleaning & Reassembly Assessment | Internal SOP | Ensures users can safely clean and reassemble without error |
Phase V: Full-Scale Production & Launch
Goal: Scale manufacturing and launch the device commercially.
Key Activities:
- Establish manufacturing processes and quality control
- Develop packaging and labeling
- Train sales and support teams
- Implement post-market surveillance plans
Milestone: Successful product launch and initial market penetration.
Note: The tests above are provided as illustrative examples to reflect the expected level of complexity and rigor required during the development of the product. Final tests, plans and protocols may vary based on the finalized design, risk assessment, and regulatory strategy.
Each phase has its own technical and business challenges, but the biggest delays typically happen when design, testing, or regulatory planning are rushed or skipped early on. By following a phased model and closing out each milestone thoroughly, you set yourself up for a smoother regulatory path, stronger manufacturing handoff, and faster market entry.
RESOURCE ALLOCATION & TEAM INVOLVEMENT
Effective development of the head holder requires coordinated contributions across multiple disciplines. Early-stage projects benefit from a lean but focused team structure that expands as complexity increases.
Core Functional Roles Required
- Inventor/Project Lead
Drives the vision, manages progress, and coordinates team efforts. - Mechanical Engineer
Designs and refines mechanical components, ensures precision and durability. - Clinical Advisor
Provides surgical expertise, validates usability, and guides clinical relevance. - Quality and Regulatory Specialist
Develops documentation, manages regulatory compliance, and plans submissions. - Manufacturing Engineer
Plans scalable production methods and supports supply chain decisions.
Specialty Support Needs
- Materials Scientist
Advises on metal selection and sterilization compatibility. - Sterilization Expert
Assesses sterilization processes and validation. - Intellectual Property Consultant
Supports patent searches and protection strategies.
| Phase | Contributors |
| Concept | Inventor, Clinical Advisor |
| Prototype | Mechanical Engineer, Inventor, Clinical Advisor |
| Testing & Validation | Mechanical Engineer, Quality/Regulatory Specialist, Sterilization Expert |
| FDA Submission | Regulatory Specialist, Inventor |
| Production & Launch | Manufacturing Engineer, Quality Specialist |
RISK MITIGATION STRATEGIES
Identifying and addressing potential risks early helps prevent costly delays or failures later in development. For a mechanical surgical device like a head holder, risks primarily center around usability, performance, mechanical safety, and regulatory compliance.
Usability Risks
- Potential Issues
- Improper securing of the patient’s head during surgery
- Complex or unintuitive adjustment mechanisms
- Difficult sterilization or reassembly post-cleaning
- Mitigation Strategies
- Involve clinical users early for feedback on prototype ergonomics
- Use human factors engineering to guide intuitive design
- Include clear instructions for setup, use, and cleaning in labeling
Performance Risks
- Potential Issues
- Mechanical instability or slippage during surgical procedures
- Loosening of fasteners over time or with repeated sterilization
- Metal fatigue or corrosion
- Mitigation Strategies
- Conduct rigorous mechanical performance testing (e.g., torque, load stability)
- Select high-strength, corrosion-resistant metals
- Simulate long-term use cycles including sterilization exposure
Mechanical Safety Risks
- Potential Issues
- Patient injury due to sharp edges or improper contact surfaces
- Device malfunction during critical surgical procedures
- Mitigation Strategies
- Ensure rounded edges and patient-safe contact areas
- Perform safety and reliability analysis during design and prototyping
- Include fail-safe mechanisms where appropriate
Regulatory Risks
- Potential Issues
- Failure to establish substantial equivalence with a predicate device
- Incomplete testing or documentation for 510(k) submission
- Mitigation Strategies
- Begin predicate device research early in development
- Maintain organized, version-controlled design documentation
- Plan a comprehensive test strategy covering mechanical and biocompatibility requirements
Manufacturing and Supply Chain Risks
- Potential Issues
- Delays or quality issues with custom-machined parts
- Inconsistent sterilization performance due to material variability
- Mitigation Strategies
- Use off-the-shelf components wherever possible
- Qualify multiple suppliers for key components
- Document sterilization validation protocols that account for process variability
Strategic Takeaway
Mitigating risks for the head holder involves a strong focus on mechanical integrity, clinical usability, and sterilization safety. Addressing these risks through early prototyping, clinical input, and robust documentation will support both regulatory success and long-term device reliability.
INVESTMENT & FINANCIAL OUTLOOK
Developing a mechanical surgical device like a head holder involves moderate financial risk but can be efficiently managed with strategic planning. Because the device is relatively simple, cost management and funding strategy are especially important to maintain a favorable development-to-return ratio.
Primary Cost Drivers
- Prototyping and Testing
Mechanical prototyping, load-bearing performance tests, and sterilization validation will be key early expenses. - Regulatory Preparation
Though a 510(k) is less expensive than a PMA, preparing a strong submission, including predicate comparison, labeling, and performance data, requires specialized input and documentation. - Clinical Engagement
Establishing relationships with clinical advisors or trial sites may involve stipends or consulting fees, especially if usability evaluations are conducted. - Manufacturing Scale-Up
Tooling and setup for precision machining, especially for a metal-based device, may require upfront investment.
Budgeting Tips for Early Inventors
- Stage investment by development phase; don’t over-invest before concept validation.
- Use virtual prototyping and CAD simulations to reduce physical prototyping cycles.
- Select off-the-shelf or easily machinable materials to reduce production costs.
- Focus initial spending on design for manufacturability (DFM) once the concept is validated.
Funding Strategy Considerations
- Explore non-dilutive funding options such as SBIR/STTR grants or institutional innovation funds.
- Consider early-stage angel investors or seed accelerators with a focus on medical devices.
- Engage potential strategic partners such as surgical equipment manufacturers who may provide development support or licensing options.
Revenue Potential Considerations
- The market favors durable, reusable devices that provide cost efficiency to hospitals.
- Revenue is typically driven by unit sales, with potential for additional income from accessories or future design variants.
- Success depends on gaining early traction through clinical endorsement and competitive pricing.
Financial Risk Mitigation
- Start with a minimal viable product (MVP) approach to limit early cash burn.
- Build a flexible supply chain to minimize production bottlenecks and price volatility.
- Conduct early market research to validate price points and purchasing behavior in target hospitals.
Strategic Takeaway
The head holder’s financial outlook is favorable for a well-managed project; its lack of electronics and moderate complexity keep costs in check. The key to success lies in capital-efficient prototyping, early regulatory planning, and validation of hospital purchasing drivers to support revenue generation.
Your Complimentary Q&A
Have questions about the report?
Book a 15-minute call to clarify insights or prioritize next steps.
Understanding Vendor Tiers and Impact on Project Cost and Time
Tier 1: Higher costs associated with comprehensive services complete system development, advanced technology, and the ability to manage complex projects. Design services may have shorter lead times due to ability to build a larger team however the scale of operations and the complexity of the more comprehensive supply chain may slow certain processes.
Tier 2: Their cost and Time may vary based on their specialization allowing for efficient production of specific components, potentially leading to shorter lead times for those items. However, since they do not provide complete systems, the overall integration into larger assemblies may require additional coordination, potentially affecting timelines.
Tier 3: Lower costs due to specialization in specific components or materials or limited staffing resources requiring additional coordination with other suppliers. This may slow the development time from both a design and supply chain perspective.
Considerations
- Despite higher costs and longer lead times, Tier 1 suppliers may be more suitable for complex projects requiring integrated solutions.
- For projects with budget constraints, engaging multiple Tier 3 suppliers could be more cost-effective, but may require more intensive project management.
- Working with Tier 3 suppliers entails coordinating a robust supply chain to ensure timely delivery and quality assurance.
The choice between Tier 1 and Tier 3 suppliers involves trade-offs between cost, time, and supply chain management complexity. Careful evaluation of project requirements and resources is essential for making an informed decision.
Disclaimers & Limitations
- Generalizations: This report provides a high-level overview based on standard assumptions and does not account for unique device characteristics. Actual costs, timelines, and risks may vary significantly depending on the device's design, use case, and target market.
- Assumptions of Device Class and Use: Assumptions were made regarding the device's classification and intended use. These assumptions can impact regulatory requirements, costs, and timelines. Specific regulatory pathways, for instance, may differ based on the device's risk classification and market entry strategy.
- Market and Regulatory Dynamics: Regulatory requirements and market conditions are subject to change. The report's cost and timeline estimates may be affected by evolving regulatory landscapes, standards, or unforeseen market dynamics, which could delay approval or require additional testing.
- Risk Assessment Limitations: Risk levels and mitigation strategies are based on general device categories and may not fully address specific technical or operational risks unique to the product. Thorough risk assessments should be tailored to the device's complexity, materials, and usage.
- Development Phases and Milestones: The development phases outlined here follow a typical medical device development pathway, but real-world project phases may overlap or require iteration due to unforeseen challenges or design changes.
- Cost and Timeline Variability: The cost and timeline estimates are based on standard industry benchmarks but do not account for project-specific adjustments. Factors like unexpected technical challenges, prototype iterations, or regulatory re-submissions can significantly impact final costs and schedules.
- Reliance on Industry Standards: The report relies on common industry standards for development and testing. However, additional standards specific to certain device features or regions may apply, affecting compliance requirements and associated timelines.
- Testing and Validation Scope: Testing and validation requirements are generalized. Devices with novel materials, complex electronics, or unique features may require additional, specialized tests, potentially extending both cost and duration.
UNLOCK NOW
- Development cost and timeline benchmarks
- Complexity insights shaping risk and effort
- Technology readiness snapshot
READY FOR EVEN MORE INSIGHTS?
Unlock for $29.95- Regulatory pathway and market opportunity
- Milestone roadmap with phase activities
- Team and resource playbook
- Risk factors and mitigation strategies
- Financial planning and commercialization outlook
.png?width=4200&height=441&name=Zewski_Report%20Logo%20(Shirts).png)