Percutaneous Catheter
ABOUT THIS REPORT
While this report focuses on the development of a Percutaneous Catheter, the insights provided are broadly applicable to similar medical devices. It's important to recognize that development timelines and costs can vary significantly between devices due to factors such as design complexity, regulatory requirements, and manufacturing processes. Nonetheless, the general principles and information outlined here offer valuable guidance for understanding the development landscape of comparable medical technologies.
DEVICE OVERVIEW
FDA Identification
A Percutaneous Catheter is a Class II medical device commonly used for therapeutic or diagnostic purposes. It is designed for minimally invasive access to the vascular or other bodily systems. The catheter is regulated under the FDA's Code of Federal Regulations (CFR) for medical devices. Most percutaneous catheters require FDA 510(k) clearance due to their intended use and potential risks, ensuring safety and effectiveness.
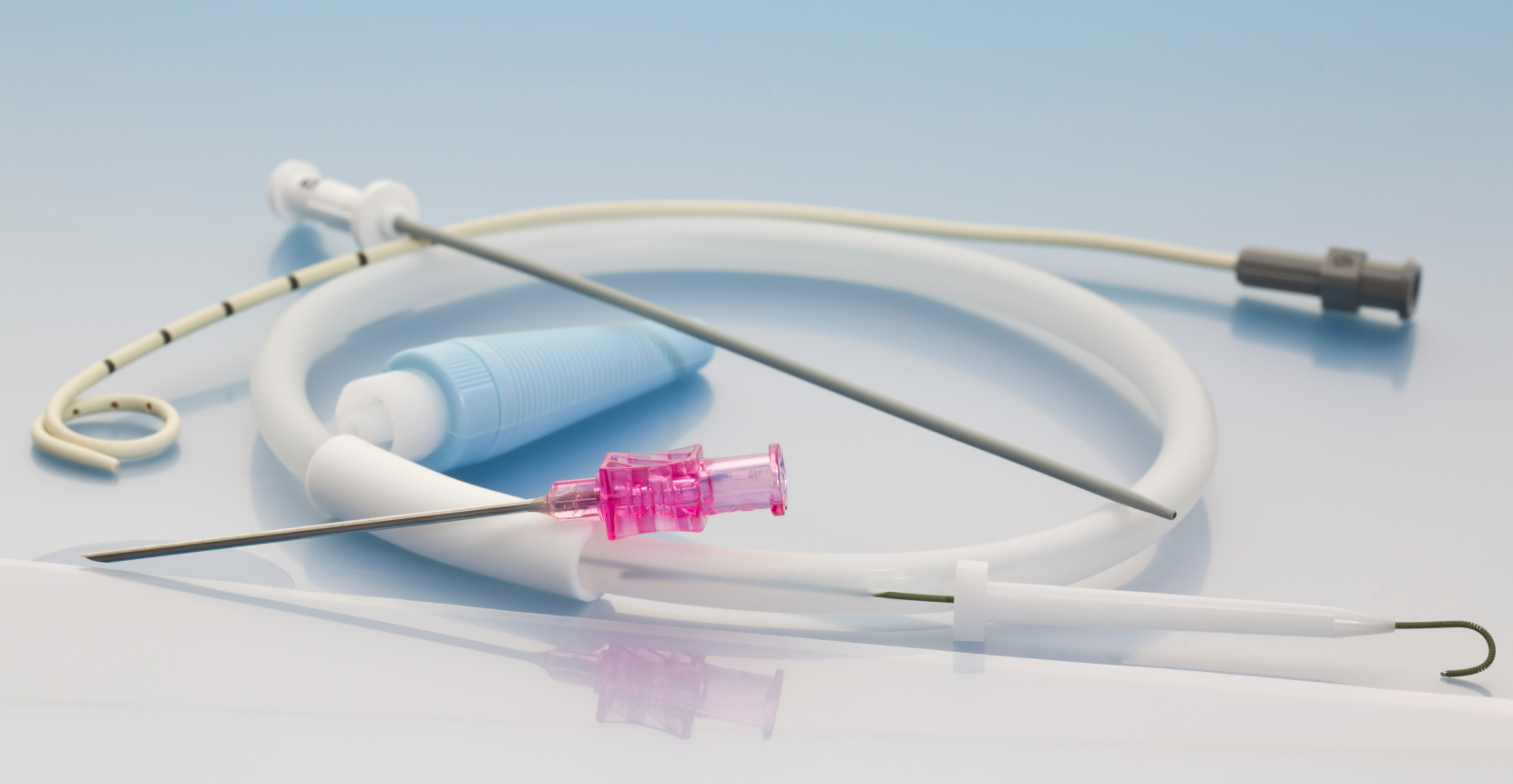
General Description
A Percutaneous Catheter is a thin, flexible medical device used for accessing blood vessels, delivering medications, or facilitating drainage during minimally invasive procedures. This device is an essential tool in interventional medicine, including cardiology, oncology, and nephrology. It is inserted through the skin (percutaneous entry) and guided to the desired location using advanced imaging techniques.
Percutaneous catheters are typically made from biocompatible materials such as medical-grade plastics and silicone, ensuring flexibility, durability, and patient safety. These materials are often combined with radiopaque markers to enhance visibility during imaging. The device may be used as part of a system, connecting to external components such as syringes, infusion pumps, or monitoring devices.
The design prioritizes sterility, ease of use, and compatibility with various clinical settings. Depending on its intended use, the catheter may include additional features such as side ports, specialized coatings to reduce friction, or integrated guidewires for enhanced maneuverability. Due to its versatility and critical role in patient care, the Percutaneous Catheter is a staple in modern medical practice.
FEASIBILITY
Understanding Your Feasibility Score
The Feasibility Score bar provides an assessment of your project’s path to market, with higher values indicating lower complexity and fewer anticipated obstacles.
- 0 - 39 (Low Feasibility): This range suggests that the project may face significant challenges due to high complexity or extensive requirements. Additional planning, resources, or risk mitigation strategies will be necessary.
- 40 - 74 (Moderate Feasibility): Projects within this range indicate a moderate path to market. While the overall complexity is manageable, some areas may require refinement or further development to ensure project stability and success.
- 75+ (High Feasibility): A score in this range indicates a relatively straightforward path to market, with low complexity and minimal additional work expected. This project is well-positioned to progress smoothly.
The Feasibility Score is a general guide, not an absolute measure of project success. We recommend using this score as part of a broader assessment and considering additional expert guidance for a comprehensive evaluation.
PROJECT OVERVIEW
Understanding your device’s purpose and intended setting is foundational to every decision you’ll make — from design and material selection to regulatory planning and commercialization strategy.
This Percutaneous Catheter is intended for therapeutic use, providing targeted treatment in clinical environments where precision, sterility, and ease of use are critical. Its ultra-compact size, flexible silicone body, and portable, handheld format suggest a strong fit for procedures requiring minimally invasive access without reliance on electronics or external power sources. These characteristics position the device for integration into a variety of workflows, including outpatient settings and bedside interventions.
At this stage, the device is still in the concept phase, and while the absence of electronics and moving parts simplifies development, the unique use of silicone and miniaturization may introduce complexities in manufacturing, testing, and cost control. These are addressed more fully in later sections, but are worth noting early as part of the broader development vision.
Moving forward, successful development will require:
- A focus on human factors engineering to ensure the catheter is intuitive to use across settings and user types.
- Strategic planning for manufacturability, as silicone components and small form factors demand high precision.
- Ongoing clinical alignment to make sure real-world needs are continuously reflected in the design.
- Foundational documentation, even at this early stage, to capture decisions, avoid rework, and support future regulatory filings.
This overview sets the stage for the device’s journey through design, testing, approval, and market launch — each phase building upon the foundation of a clearly defined and well-understood clinical purpose.
COST & TIME ESTIMATES
DEVELOPMENT COMPLEXITY
At first glance, your device appears mechanically simple — no electronics, no moving parts, and no advanced environmental requirements like waterproofing or heat resistance. But development complexity isn’t just about what a device does. It’s also shaped by how well the design supports future production, and how early decisions can ripple through the project in unexpected ways.
What Simplifies Development
- No power or software requirements eliminates firmware integration, electrical safety validation, and cybersecurity risk
- No moving parts reduces the need for mechanical endurance testing or fatigue modeling
- No heat/water resistance requirements remove the need for specialized materials or multi-phase validation
- These attributes lower the technical barriers to entry and shorten the list of required performance tests.
What Introduces Complexity (and Cost)
Use of Silicone- Silicone is an excellent material for comfort, biocompatibility, and flexibility — but it’s not trivial to manufacture. It often requires:
- Specialized tooling for liquid injection molding (LIM) or compression molding
- Longer curing times and tighter environmental controls
- Design adjustments to reduce flash, air entrapment, or warping
If DFM (Design for Manufacturability) hasn't been considered yet, even a small design change (e.g. wall thickness, taper, or port location) could significantly affect tooling costs or defect rates.
Miniaturization & Tolerance RiskBecause your catheter is very small, even slight design variances can result in big performance differences — especially for inner lumens, connectors, or bond points. This increases:
- The need for precision tooling
- Difficulty in inspection and QA
- Sensitivity to material shrinkage or warping
If tight tolerances aren’t designed with manufacturing in mind, the result can be unnecessary scrap, rework, or tooling redesign.
No Early DFM Integration- You’ve indicated that DFM has not been applied yet. This is typical for early-stage concepts, but it means:
- Design decisions made now may not align with real-world manufacturing constraints
- The risk of expensive redesign increases during prototyping and testing
- Vendors may reject or heavily modify your design during quote review
This doesn’t mean the concept is flawed — just that proactive DFM review during early CAD stages can reduce future surprises and compress your timeline later on.
Strategic Takeaway
Your device benefits from a low baseline complexity — but material choices, precision requirements, and the absence of DFM planning introduce hidden risks. These factors may not show up in prototyping, but they can increase cost, delay, or failure rate during testing or early manufacturing.
Now is the time to partner with a design engineer or manufacturer who can help you bridge the gap between what you envision and what can be built reliably at scale.
TECHNOLOGICAL READINESS
At this stage, your device is in its conceptual phase — a critical early point in development where ideas begin to take shape, but have yet to be translated into physical prototypes or formal design documentation.
While early-stage concepts offer creative flexibility, they also present a few key challenges:
- There’s no physical prototype yet to test or evaluate
- The design hasn’t been iterated based on feedback or real-world constraints
- Core documentation (e.g. design inputs, outputs, traceability matrix) is still to be developed
- No intellectual property protections are in place to guard against competitors
These factors are common at this phase and not a cause for concern — but they do signal that foundational steps are still ahead. Taking time now to explore the device’s clinical value, technical feasibility, and intended workflow will prevent costly pivots later.
Key Next Steps to Advance Technological Maturity
- Sketch to Prototype: Begin translating your concept into basic CAD models or early prototypes. These don’t need to be final — they’re tools to ask better questions and test assumptions.
- Early Risk Review: Identify potential technical and clinical risks (e.g. insertion ease, catheter kinking, material compatibility) even before formal design work begins.
- Document as You Go: Start capturing design decisions, constraints, and open questions. Even informal notes now can lay the groundwork for required regulatory documentation later.
- Initiate an IP Strategy: Consider a provisional patent filing to secure early protection, especially if you plan to discuss the concept with external partners, clinicians, or investors.
- Validate Clinical Relevance: Continue conversations with your clinical contact and begin identifying target users and care settings. Their feedback can shape design priorities and reduce unnecessary features.
Technological readiness is not about being “finished” — it’s about having enough clarity to move forward with confidence. By investing time in structured thinking and light-touch testing now, you’ll avoid rework later and accelerate development when resources come into play.
REGULATORY APPROVAL
Understanding the regulatory path early on is key to keeping your device on track for market entry — and avoiding costly surprises later.
Based on your device’s characteristics, it would likely be classified as a Class II medical device, which places it in the moderate-risk category. This means you’ll need to pursue a 510(k) submission to gain FDA clearance. The goal of this process is to show that your device is substantially equivalent to an existing, legally marketed product — known as a predicate device.
While this pathway is more streamlined than a full Premarket Approval (PMA), it still requires careful planning, documentation, and testing.
FDA Classification Snapshot
- Regulation Number: 870.1250
- Product Code: DQY
- Regulation Medical Specialty: Cardiovascular
- Device Class: Class II
- Submission Pathway: 510(k) Premarket Notification
You should work with a regulatory consultant to verify the correct classification and any associated guidance documents.
What the 510(k) Process Involves
- Device Description & Intended Use: You’ll need to clearly define what the device does, who it’s for, and how it’s used.
- Substantial Equivalence: You must compare your device to a predicate with similar design, materials, performance, and intended use.
- Performance Testing: Bench testing must show that your device operates reliably and safely under expected conditions.
- Biocompatibility Testing: Since the catheter is moderately invasive, you’ll need to evaluate cytotoxicity, irritation, and sensitization risk.
- Sterility & Shelf-Life Validation: As a disposable, single-use device, you’ll validate the sterile barrier system but won’t need to submit cleaning or reuse protocols.
Why Your Path Is Streamlined
Your device benefits from a number of development and regulatory simplifications:
- No electronics or software = no electrical safety or cybersecurity requirements
- No power source = no battery or charging risks
- No moving parts = fewer failure modes and simplified mechanical testing
- Disposable design = no reprocessing validation or use-life studies required
What to Do Now
- Find a Predicate Device: Search FDA databases or past 510(k) summaries for similar catheters.
- Start a Test Plan: Draft a list of performance, packaging, and biocompatibility tests you’ll need.
- Outline Required Documentation: Begin building your design history file (DHF) structure—even with placeholders.
- Consider Early Consultation: Engaging a regulatory advisor early can save time and reduce rework.
The 510(k) process is manageable — but it rewards preparation. By aligning your design and testing strategy early, you can streamline submission and minimize regulatory delays.
MARKET POTENTIAL
Bringing a new medical device to market isn’t just about technical feasibility — it’s about proving that the product solves a meaningful problem in a way the market cares about. For early-stage inventors, understanding the market landscape helps ensure you're building something both clinically valuable and commercially viable.
Your device — a very small, disposable percutaneous catheter for therapeutic use — may occupy a niche space within interventional care, vascular access, or localized drug delivery. While the concept introduces incremental improvements over existing devices (such as size, flexibility, or ease of use), those subtle upgrades can be compelling in the right clinical and economic context.
What Boosts Your Market Potential
- Single-use design: Streamlines procurement and eliminates sterilization burden for facilities
- Compact, ergonomic format: Increases usability in outpatient or bedside settings
- Material flexibility (e.g. silicone): Enhances comfort and reduces risk of tissue trauma
- Slight feature differentiation: Could appeal to clinicians frustrated by current limitations in maneuverability, compatibility, or patient tolerance
Market Entry Factors to Plan For
- Reimbursement Landscape: If your device is used in a reimbursed procedure (e.g. vascular access, drainage, pain management), it may benefit from existing billing codes — but you'll need to validate this with payers.
- Clinical Buying Decision: In most care settings, clinicians don’t buy the product directly. Purchasing decisions are often made by supply chain managers, clinical committees, or hospital administrators. Your value proposition must speak to cost-effectiveness and workflow integration, not just performance.
- Customization Expectations: If targeting global or multi-specialty markets, slight adjustments to packaging, catheter length, or compatibility may improve adoption without requiring a full redesign.
How to Strengthen Market Viability from Day One
- Talk to Buyers, Not Just Users: Clinicians may love the concept, but procurement teams care about inventory costs, shelf life, and interchangeability.
- Review Competitor Weak Spots: Identify what frustrates current users of similar catheters — your innovation sweet spot might be hiding in a minor workflow improvement.
- Stay Scalable: Your concept is inherently simple, which is a strength — minimize complexity unless the added value justifies it.
- Start Lightweight Market Validation: Even informal conversations with 3–5 clinicians and 1 hospital procurement manager can shape your go-to-market plan dramatically.
You don’t need to have all the answers now — but being aware of how your product fits into real-world clinical and commercial workflows helps shape smarter decisions as development progresses.
DEVELOPMENT PHASES & MILESTONES
Bringing a medical device from concept to market involves distinct phases — each with its own goals, decisions, and milestones. While timelines and activities vary by project, the following roadmap outlines a typical path for a Class II, single-use therapeutic catheter like yours.
Each phase builds on the last, helping you reduce risk, validate assumptions, and gather the data needed for regulatory approval and market readiness.
Phase I: Concept Development
Goal: Establish feasibility and define the problem your device solves.
Key Activities:
- Identify user needs and key clinical use cases
- Sketch out design ideas and system components
- Begin early market research and predicate device analysis
- Seek clinical feedback to refine value proposition
- Explore basic materials and device configurations
Milestone: Defined product concept and high-level requirements.
Phase II: Prototype Development
Goal: Create a physical representation of the idea for testing and feedback.
Key Activities:
- Develop CAD models and 3D-printed or molded prototypes
- Begin bench-level performance testing
- Assess manufacturability of the initial design
- Collect structured user feedback on form, fit, and usability
Milestone: Functional prototype ready for refinement and verification planning.
Phase III: Design Output & Verification
Goal: Prove the device works as intended, safely and reliably.
Key Activities:
- Conduct verification testing (does it meet design specs?)
- Perform biocompatibility and material safety testing
- Refine labeling, packaging, and instructions for use
- Begin documentation for FDA submission (Design History File)
Milestone: Completed test reports to support regulatory clearance.
Performance Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Dimensional Verification | Internal SOP or ISO 10555 | Confirms consistency of key physical dimensions |
| Flow Rate / Pressure Testing | ISO 10555-1 | Validates delivery function under expected conditions |
| Tensile / Pull-out Force | ISO 10555-1 or ASTM F88 | Ensures catheter will not detach during use |
| Kink Resistance / Flexural Strength | ASTM D790 or ISO 178 | Ensures performance during bending or insertion |
| Leak / Burst Pressure Testing | ISO 10555-1 or ISO 80369 | Confirms device integrity and safety under pressure |
| Connection Compatibility (luer lock, etc.) | ISO 80369 series | Confirms connection safety with standard components |
Biocompatibility Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Cytotoxicity | ISO 10993-5 | Screens for cell toxicity |
| Sensitization | ISO 10993-10 | Assesses potential allergic reactions |
| Irritation or Intracutaneous Reactivity | ISO 10993-10 | Tests for tissue inflammation |
| Systemic Toxicity (acute) | ISO 10993-11 | Evaluates short-term exposure effects |
| Material Characterization (Extractables / Leachables) | ISO 10993-18 / 17 | Identifies chemical compounds in contact with body |
| Optional: Hemocompatibility | ISO 10993-4 | Recommended if used in vascular access |
Sterility & Packaging Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Packaging Seal Integrity | ASTM F1929, F88 | Ensures sterile barrier integrity |
| Packaging Aging / Shelf-Life | ASTM F1980 (accelerated aging) | Predicts packaging durability over time |
| Sterility Assurance (SAL 10⁻⁶) | ISO 11137 (EtO / gamma) or ISO 11737 | Confirms sterility level and validation method |
| Bioburden & Sterility Testing | SO 11737-1 / -2 | Validates initial microbial load & sterilization |
Phase IV: Validation & Regulatory Submission
Goal: Submit a 510(k) package and receive FDA clearance.
Key Activities:
- Finalize all design, risk, and testing documentation
- Identify and describe a suitable predicate device
- Compile and submit your 510(k) to the FDA
- Respond to any feedback or requests for additional information
Milestone: FDA clearance to market the device.
510(k) Submissions Guidance - Catheters
Usability & Labeling Matrix
| Test Name | Standard / Reference | Purpose |
| Human Factors Review (basic risk-based) | FDA Guidance (IEC 62366) | Ensures instructions and labeling minimize user error |
| Label Legibility & Durability | Internal SOP / ISTA standards | Required for shelf life and packaging validation |
Phase V: Full-Scale Production & Launch
Goal: Prepare for commercial production and distribution.
Key Activities:
- Finalize suppliers and production tooling
- Conduct pilot production runs and implement quality systems
- Establish packaging and sterilization workflows
- Launch sales and marketing efforts in targeted channels
Milestone: Product commercially available and supported in-market.
RESOURCE ALLOCATION & TEAM INVOLVEMENT
Even a seemingly simple device like a therapeutic catheter demands contributions from a diverse team across design, testing, manufacturing, and regulatory approval. While early-stage inventors often wear many hats at first, building awareness of key roles and responsibilities early on can help streamline development and avoid critical gaps down the road.
Core Teams
- Engineering & Design
- Role: Develops CAD models, selects materials, builds prototypes, and ensures the device meets performance and usability requirements.
- What to Plan For: Even without electronics or moving parts, miniaturization and silicone molding demand precision design and manufacturing coordination.
- Regulatory & Compliance
- Role: Defines the regulatory strategy, ensures testing aligns with FDA expectations, and prepares your 510(k) submission.
- What to Plan For: This team tracks standards, guides documentation, and interprets regulatory feedback — essential for Class II devices.
- Manufacturing & Quality
- Role: Builds the physical product at scale, ensures component quality, and manages production tolerances and tooling.
- What to Plan For: Silicone molding, material traceability, and sterile packaging all require tight quality control and experienced vendors.
- Supply Chain & Procurement
- Role: Sources off-the-shelf and custom components, coordinates with suppliers, and manages timelines for materials.
- What to Plan For: Supply chain complexity increases when using specialty materials (like medical-grade silicone) or when lead times fluctuate.
- Project Management
- Role: Oversees development milestones, timelines, team communication, and risk mitigation across all phases.
- What to Plan For: Especially helpful when juggling external vendors, part iterations, or parallel activities like testing and documentation.
| Phase | Contributors |
| Concept | Inventor, Clinical Advisor |
| Prototype | Design Engineer, Materials Specialist |
| Testing & Validation | QA/RA Lead, Test Lab Partner |
| FDA Submission | Regulatory Consultant or In-House RA Lead |
| Production & Launch | Manufacturing Engineer, Supplier Coordinator, Sales/Marketing Advisor |
Building a successful product isn’t about hiring a massive team up front — it’s about knowing when to bring in the right expertise, and how to keep communication clear between stakeholders. Even a few strategic collaborators can dramatically increase your speed and confidence through development.
RISK MITIGATION STRATEGIES
Every medical device project carries risks — but the goal isn’t to eliminate them all. It’s to identify the most likely challenges early, so you can reduce their impact with smart planning, testing, and collaboration.
For your concept-stage catheter — simple in function but highly regulated — risks fall into three main categories: technical, regulatory, and manufacturing.
Technical Risks
Miniaturization Tolerances
- Very small devices leave less room for design errors. Even small deviations in lumen size or wall thickness can affect flow rate, structural integrity, or user handling.
- Mitigation: Use high-resolution prototyping methods early. Tolerance stack-up should be reviewed as soon as the first CAD model is developed.
Material Compatibility
- Silicone is biocompatible but can degrade under certain conditions or bond poorly with other components.
- Mitigation: Conduct accelerated aging and bonding tests during prototyping. Validate material sourcing early to avoid late-stage redesign.
Lack of Iteration
- With no prior prototypes, assumptions may go untested.
- Mitigation: Treat early prototypes as learning tools — not final versions. Budget time for at least one refinement cycle before entering verification testing.
Regulatory Risks
Insufficient Testing Scope
- Many first-time inventors underestimate the breadth of testing required for Class II devices — especially for biocompatibility and packaging validation.
- Mitigation: Work with a regulatory consultant to map out all required tests upfront (ISO 10993, ISO 11607, etc.). Incorporate this into your design and budget plans.
Predicate Mismatch
- Choosing a poor predicate can trigger FDA questions or additional submission delays.
- Mitigation: Research past 510(k) clearances early. Choose a predicate with a similar intended use, construction, and patient-contact profile.
Lack of Documentation
- Even if your device is simple, the FDA expects thorough design history files, risk assessments, and labeling controls.
- Mitigation: Start lightweight documentation now, even before design finalization. Capturing rationale and design intent early helps avoid rework.
Manufacturing Risks
Custom Silicone Molding
- Producing medical-grade silicone parts requires tight process control. Flash, poor bonding, or inconsistent curing can affect performance.
- Mitigation: Vet suppliers carefully and request small trial runs. Partner with a molder experienced in small-lumen medical components.
Supply Chain Volatility
- Custom components or specialty materials can create long lead times or sourcing gaps.
- Mitigation: Identify off-the-shelf alternatives where possible. Lock in vendor timelines and have a backup plan before final design freeze.
Risk Level Summary
Your overall project risk is moderate: low in complexity, but high in precision, documentation, and regulatory expectation. Addressing these areas early will reduce the likelihood of costly redesigns or submission delays.
INVESTMENT & FINANCIAL OUTLOOK
Launching a medical device isn’t just a technical journey—it’s a financial one. Understanding the funding requirements and financial risks of your project from the outset helps you plan smarter, avoid surprises, and attract the right partners.
Your device—a Class II, single-use therapeutic catheter—sits at the lower-to-moderate end of the development cost spectrum. It’s mechanically simple and doesn’t require electronics, software, or sterilization reprocessing protocols. However, it’s still subject to stringent regulatory, biocompatibility, and quality requirements, which drive the bulk of development costs.
Estimated Development Costs
Each phase of development incurs specific costs related to design, testing, documentation, and compliance. Your total development investment will depend on:
- Prototyping method (3D printing vs. molded samples)
- Number of iterations before locking design
- Testing scope (e.g., full ISO 10993 biocompatibility panel)
- Regulatory consulting and submission prep
- Tooling for full-scale production
Market Revenue Potential
Because your product introduces slight functional improvements over existing devices, it’s not positioned as disruptive—but it could offer an efficiency edge or comfort advantage that appeals to niche markets or under-addressed clinical frustrations.
Disposable design and minimal customization needs also make it easier to scale once cleared, as the unit cost can decrease significantly with volume.
Funding Strategy Considerations
You don’t need a massive fundraise to get started—but a staged approach to capital will help you move efficiently from concept to clearance:
- Pre-seed: Early design, prototyping, and clinical input (bootstrap, angel investors, or grants)
- Seed round: Regulatory planning, verification testing, and 510(k) submission (VCs, medtech accelerators, SBIR grants)
- Series A or strategic partnership: Scaling manufacturing, commercialization, and market entry
Disposable medical devices often appeal to investors seeking predictable manufacturing, fast-turn inventory, and repeat sales potential—especially if the bill of materials is low and the use case is tied to reimbursed procedures.
Financial Risk Mitigation
To avoid budget overruns or funding gaps:
- Start cost tracking now—even if estimates are rough
- Build in 10–20% buffer for unforeseen redesigns or test failures
- Use phased milestones to align funding tranches with clear progress (e.g. prototype completed, submission filed, clearance granted)
- Explore non-dilutive funding sources like National Institutes of Health (NIH) grants, Biomedical Advanced Research and Development Authority (BARDA), or state innovation funds
A solid financial plan doesn’t just unlock development—it signals to partners and investors that you’re serious about making your vision real, responsibly.
Understanding Vendor Tiers and Impact on Project Cost and Time
Tier 1: Higher costs associated with comprehensive services complete system development, advanced technology, and the ability to manage complex projects. Design services may have shorter lead times due to ability to build a larger team however the scale of operations and the complexity of the more comprehensive supply chain may slow certain processes.
Tier 2: Their cost and Time may vary based on their specialization allowing for efficient production of specific components, potentially leading to shorter lead times for those items. However, since they do not provide complete systems, the overall integration into larger assemblies may require additional coordination, potentially affecting timelines.
Tier 3: Lower costs due to specialization in specific components or materials or limited staffing resources requiring additional coordination with other suppliers. This may slow the development time from both a design and supply chain perspective.
Considerations
- Despite higher costs and longer lead times, Tier 1 suppliers may be more suitable for complex projects requiring integrated solutions.
- For projects with budget constraints, engaging multiple Tier 3 suppliers could be more cost-effective, but may require more intensive project management.
- Working with Tier 3 suppliers entails coordinating a robust supply chain to ensure timely delivery and quality assurance.
The choice between Tier 1 and Tier 3 suppliers involves trade-offs between cost, time, and supply chain management complexity. Careful evaluation of project requirements and resources is essential for making an informed decision.
Disclaimers & Limitations
- Generalizations: This report provides a high-level overview based on standard assumptions and does not account for unique device characteristics. Actual costs, timelines, and risks may vary significantly depending on the device's design, use case, and target market.
- Assumptions of Device Class and Use: Assumptions were made regarding the device's classification and intended use. These assumptions can impact regulatory requirements, costs, and timelines. Specific regulatory pathways, for instance, may differ based on the device's risk classification and market entry strategy.
- Market and Regulatory Dynamics: Regulatory requirements and market conditions are subject to change. The report's cost and timeline estimates may be affected by evolving regulatory landscapes, standards, or unforeseen market dynamics, which could delay approval or require additional testing.
- Risk Assessment Limitations: Risk levels and mitigation strategies are based on general device categories and may not fully address specific technical or operational risks unique to the product. Thorough risk assessments should be tailored to the device's complexity, materials, and usage.
- Development Phases and Milestones: The development phases outlined here follow a typical medical device development pathway, but real-world project phases may overlap or require iteration due to unforeseen challenges or design changes.
- Cost and Timeline Variability: The cost and timeline estimates are based on standard industry benchmarks but do not account for project-specific adjustments. Factors like unexpected technical challenges, prototype iterations, or regulatory re-submissions can significantly impact final costs and schedules.
- Reliance on Industry Standards: The report relies on common industry standards for development and testing. However, additional standards specific to certain device features or regions may apply, affecting compliance requirements and associated timelines.
- Testing and Validation Scope: Testing and validation requirements are generalized. Devices with novel materials, complex electronics, or unique features may require additional, specialized tests, potentially extending both cost and duration.
.png?width=4200&height=441&name=Zewski_Report%20Logo%20(Shirts).png)
