Apnea Monitor
Device Type: Anesthesiology - Monitoring
FDA Description:
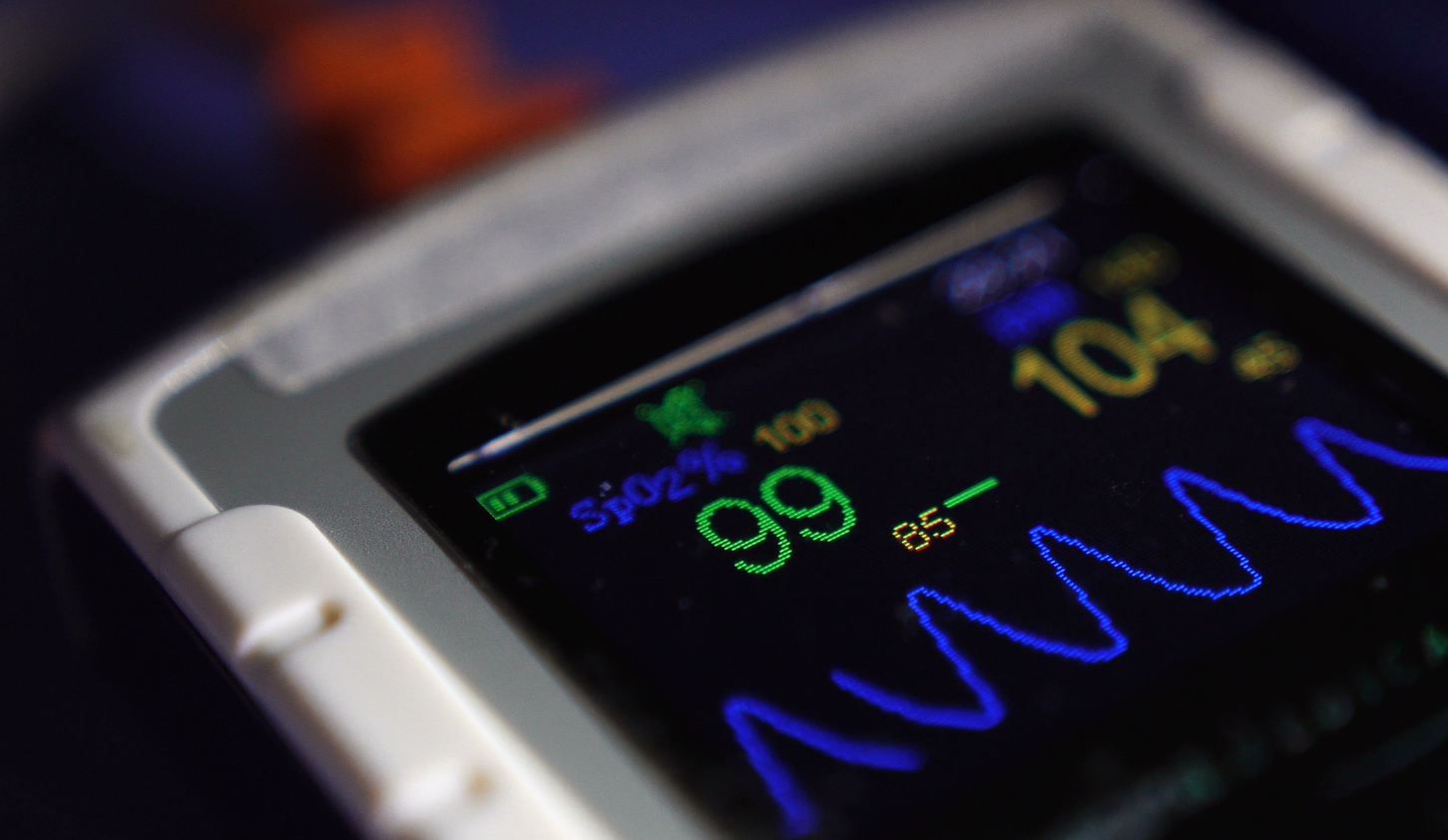
An apnea monitor is a Class II medical device designed to alert users to the cessation of breathing, typically timed from the last detected breath. It may also monitor indirect indicators such as heart rate and other physiological parameters associated with respiration. The FDA product code for an apnea monitor is FLS.
General Description:
An apnea monitor is a medical device designed to detect and alert users to instances of apnea, a temporary cessation of breathing. Commonly used for infants, adults with sleep apnea, or patients in critical care, these monitors play a vital role in early detection and intervention. They continuously track respiratory activity and often measure related physiological parameters, such as heart rate or oxygen saturation, depending on the device type.
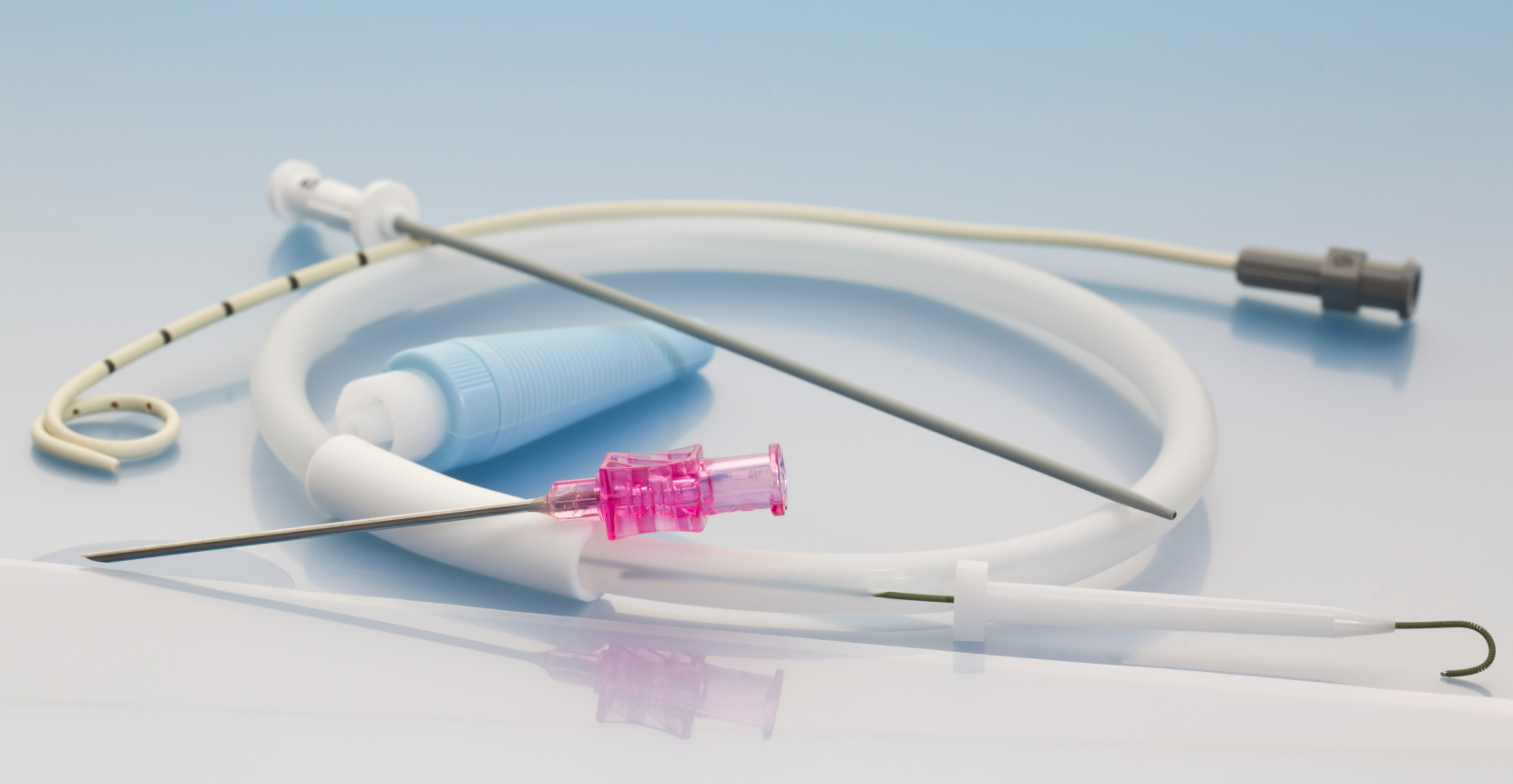
The device typically consists of sensors placed on the patient’s chest or abdomen to monitor breathing movements or airflow. In the case of neonatal apnea monitors, these are often paired with sensitive electrodes or belts that detect small chest wall movements. If breathing ceases for a predetermined period, the monitor triggers an audible or visual alarm to alert caregivers or medical staff.
Modern apnea monitors often integrate advanced features like wireless connectivity, allowing real-time data tracking through mobile apps or central monitoring systems. This facilitates remote patient monitoring and data analysis for long-term care management.
Engineered for safety and reliability, apnea monitors meet stringent regulatory standards, including FDA requirements, to ensure accurate performance. They are used in home, clinical, and neonatal intensive care settings, providing critical support for patients at risk of respiratory complications.
Apnea Monitor
General Report
Project Overview
Cost & Time Estimates
Development Complexity
Technological Readiness
Regulatory Approval
Market Potential
Development Phases & Milestones
Resource Allocation & Team Involvement
Risk Mitigation Strategies
Investment & Financial Outlook
Feasibility
Understanding Your Feasibility Score
The Feasibility Score bar provides an assessment of your project’s path to market, with higher values indicating lower complexity and fewer anticipated obstacles.
- 0 - 39 (Low Feasibility): This range suggests that the project may face significant challenges due to high complexity or extensive requirements. Additional planning, resources, or risk mitigation strategies will be necessary.
- 40 - 74 (Moderate Feasibility): Projects within this range indicate a moderate path to market. While the overall complexity is manageable, some areas may require refinement or further development to ensure project stability and success.
- 75+ (High Feasibility): A score in this range indicates a relatively straightforward path to market, with low complexity and minimal additional work expected. This project is well-positioned to progress smoothly.
The Feasibility Score is a general guide, not an absolute measure of project success. We recommend using this score as part of a broader assessment and considering additional expert guidance for a comprehensive evaluation.
Cost & Time Breakdown
Phase I
Phase II
Phase III
Phase IV
Phase V
Disclaimers & Limitations
- Generalizations: This report provides a high-level overview based on standard assumptions and does not account for unique device characteristics. Actual costs, timelines, and risks may vary significantly depending on the device's design, use case, and target market.
- Assumptions of Device Class and Use: Assumptions were made regarding the device's classification and intended use. These assumptions can impact regulatory requirements, costs, and timelines. Specific regulatory pathways, for instance, may differ based on the device's risk classification and market entry strategy.
- Market and Regulatory Dynamics: Regulatory requirements and market conditions are subject to change. The report's cost and timeline estimates may be affected by evolving regulatory landscapes, standards, or unforeseen market dynamics, which could delay approval or require additional testing.
- Risk Assessment Limitations: Risk levels and mitigation strategies are based on general device categories and may not fully address specific technical or operational risks unique to the product. Thorough risk assessments should be tailored to the device's complexity, materials, and usage.
- Development Phases and Milestones: The development phases outlined here follow a typical medical device development pathway, but real-world project phases may overlap or require iteration due to unforeseen challenges or design changes.
- Cost and Timeline Variability: The cost and timeline estimates are based on standard industry benchmarks but do not account for project-specific adjustments. Factors like unexpected technical challenges, prototype iterations, or regulatory re-submissions can significantly impact final costs and schedules.
- Reliance on Industry Standards: The report relies on common industry standards for development and testing. However, additional standards specific to certain device features or regions may apply, affecting compliance requirements and associated timelines.
- Testing and Validation Scope: Testing and validation requirements are generalized. Devices with novel materials, complex electronics, or unique features may require additional, specialized tests, potentially extending both cost and duration.
- Supplier Chain for Complex Equipment: If your device includes advanced 'add-in' equipment like sensors, lasers, pumps, or vision systems, etc., the development timeline and associated costs will require a custom report.
.png?width=4200&height=441&name=Zewski_Report%20Logo%20(Shirts).png)