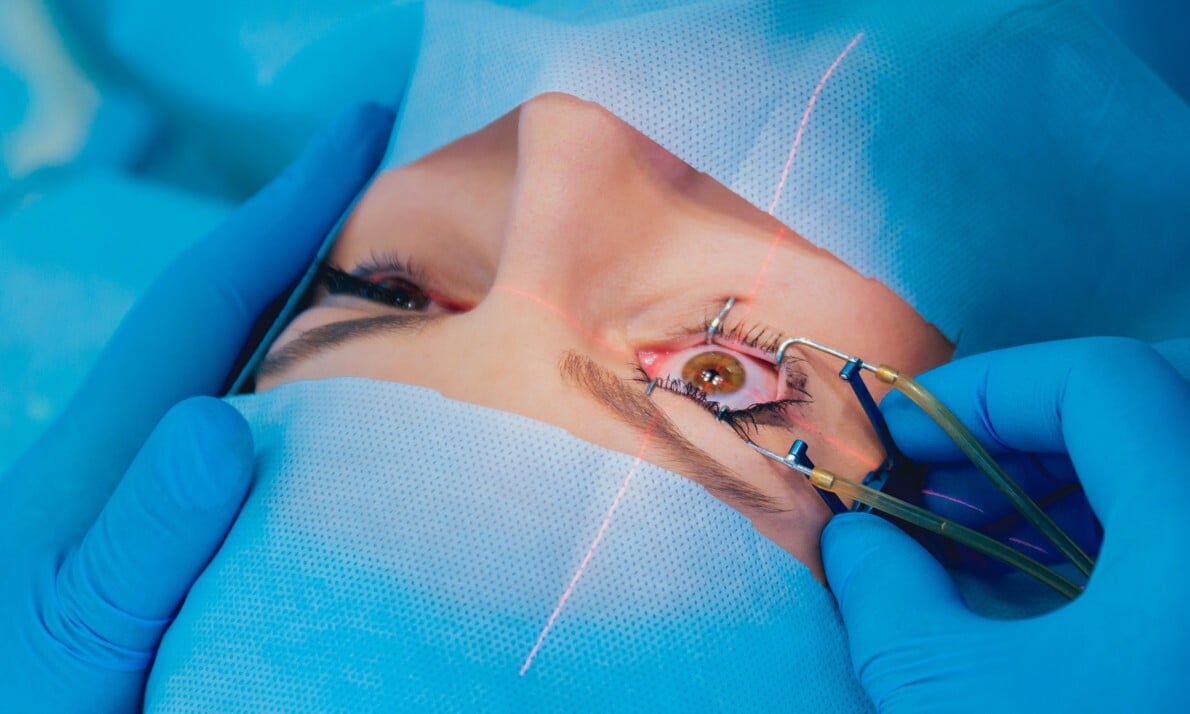
Image is for illustrative purposes only.
Ophthalmic Speculum, or Similar
GETTING STARTED
This report is a roadmap preview for an Ophthalmic Speculum – not a custom plan. It’s framed as if starting from scratch, highlighting the typical development steps, costs, and hurdles common to devices in this category. Use it to find patterns that apply to your project even if features differ.
As you read:
Look for parallels with your own concept.
Pay attention to phase transitions – that’s where costs and timelines often shift.
Use the benchmarks as reference points, not exact budgets or schedules.
Share it with partners or investors to set realistic expectations from the start.
The aim is to show likely complexities early so you can plan with confidence.
DEVICE OVERVIEW
The ophthalmic speculum is a handheld surgical instrument designed to hold the eyelids apart during ophthalmic procedures. Typically constructed from stainless steel or other sterilizable metals, this tool ensures consistent access to the eye while minimizing the need for manual assistance from a second operator. It plays a critical role in eye surgeries such as cataract extraction, retinal repair, and corneal transplantation, where maintaining a clear and unobstructed field is essential for precision.
As a manual, non-powered device with simple mechanical elements, the ophthalmic speculum is generally comprised of two arms that expand outward when actuated, using a spring or screw mechanism. Depending on the design, these mechanisms can vary in complexity, from basic spring-loaded systems to adjustable screw-operated models that allow for variable tension and retraction.
Because it interfaces directly with the ocular region, the ophthalmic speculum must be biocompatible, easy to sterilize, and resistant to corrosion from repeated autoclave cycles. Given its frequent use in high-precision, sterile environments, its design must also prioritize user ergonomics and patient comfort.
This device falls under the FDA’s general classification of manual ophthalmic surgical instruments, alongside instruments like ophthalmic forceps, iris retractors, and lachrymal dilators. While the function of the speculum is straightforward, its consistent performance and compatibility with delicate ocular procedures are vital for successful surgical outcomes.
Strategic Takeaway
The ophthalmic speculum, though mechanically simple, occupies a critical position in ophthalmic surgery. Its design must emphasize reliability, reusability, and comfort for both surgeon and patient. As a Class I manual instrument, it offers a relatively streamlined regulatory path, but design precision and manufacturing consistency remain key to market success.
FEASIBILITY
Understanding Your Feasibility Score
The Feasibility Score bar provides an assessment of your project’s path to market, with higher values indicating lower complexity and fewer anticipated obstacles.
- 0 - 39 (Low Feasibility): This range suggests that the project may face significant challenges due to high complexity or extensive requirements. Additional planning, resources, or risk mitigation strategies will be necessary.
- 40 - 74 (Moderate Feasibility): Projects within this range indicate a moderate path to market. While the overall complexity is manageable, some areas may require refinement or further development to ensure project stability and success.
- 75+ (High Feasibility): A score in this range indicates a relatively straightforward path to market, with low complexity and minimal additional work expected. This project is well-positioned to progress smoothly.
The Feasibility Score is a general guide, not an absolute measure of project success. We recommend using this score as part of a broader assessment and considering additional expert guidance for a comprehensive evaluation.
PROJECT OVERVIEW
Current Position in the Development Journey
The ophthalmic speculum project is currently in the concept phase, with a working idea or proof-of-concept in place. At this early stage, the core functionality has likely been outlined, and initial feedback from a clinical supporter has helped shape the direction of the design. However, the project has not yet undergone iterative prototyping, detailed documentation, or structured engineering analysis.
The absence of design-for-manufacture (DFM) considerations and the lack of formal technical documentation suggest that the project is still pre-engineering. This is a normal position for early inventors, particularly for simple mechanical devices, and offers a clean slate for setting up development processes correctly from the start.
Uniqueness and Context
This project presents a slightly unique take on a well-established device. Since ophthalmic specula are widely used in eye surgery, entering this market will require a clear articulation of what differentiates this design, whether it’s improved ergonomics, material performance, retraction force adjustability, or compatibility with specialized surgical procedures.
With one patent granted and no litigation risks, the project benefits from some initial intellectual property positioning. The scope is limited to a single country, which suggests future plans could include filing internationally or adapting the design for various regional regulatory needs.
From a clinical engagement standpoint, there is support from a champion, but not a full partnership. This means there’s an opportunity to deepen that relationship, perhaps by involving the clinical advisor in early usability testing or feedback sessions during prototyping.
What Lies Ahead
Several foundational activities still need to be addressed. The team must:
- Define core design requirements and risk-based specifications.
- Begin developing and iterating physical prototypes.
- Document design inputs and outputs to support regulatory readiness.
- Prepare for verification and biocompatibility testing.
- Align the design with sterilization requirements and mechanical safety standards.
- Evaluate manufacturing strategies for reusability and production cost-efficiency.
Because this is a reusable, sterilizable surgical instrument, later-stage planning must include thorough validation of cleaning, disinfection, and sterilization protocols. Additionally, while electronics are not involved, simple mechanical parts still require tolerance evaluation, hinge durability assessments, and user safety considerations.
Strategic Takeaway
This project is in a strong position to begin structured development, with early IP protection and clinical support already in place. The lack of iterations and technical documentation points to an important opportunity: by setting up formal development and testing workflows now, the team can avoid downstream delays and accelerate a smooth transition to regulatory and market phases.
COST & TIME ESTIMATES
DEVELOPMENT COMPLEXITY
Developing an ophthalmic speculum may seem straightforward due to its simple mechanical nature, but even low-tech surgical tools involve a mix of design precision, material science, usability testing, and regulatory diligence. Understanding what simplifies development, and what introduces complexity, can help guide decisions and prevent unexpected slowdowns or cost overruns.
Primary Drivers of Complexity
Even though the device contains no electronics or power systems, there are several key elements that add technical and operational complexity:
- Reusability with Sterilization
Devices intended for reuse in sterile environments must withstand repeated autoclave cycles. This requires careful material selection (typically surgical-grade stainless steel) and consideration of component fatigue or corrosion over time. - Intraoperative Functionality
The device must function flawlessly during surgery without requiring readjustment. Any stiffness, misalignment, or spring failure could disrupt delicate procedures, so mechanical tolerances and fatigue resistance must be tightly controlled. - Moderate Invasiveness
While the device does not enter the eye, it does directly contact sensitive tissue (eyelids, lashes, surrounding ocular region). This introduces usability risks and biocompatibility requirements that cannot be overlooked. - Custom Supply Chain Components
While many ophthalmic specula share standardized shapes, any design modifications (such as special tension mechanisms or geometry optimizations) can require custom machining or tooling, increasing manufacturing lead time and cost.
What Simplifies Development
Several attributes of the project help reduce complexity compared to more advanced surgical tools:
- No Electronics or Software
Without sensors, controls, or digital components, there’s no need for software validation, electromagnetic interference testing, or battery integration, significantly reducing regulatory burdens. - Small Size and Simplicity
The device is compact and manually operated. Once the mechanical performance is validated, the focus can shift to optimizing ergonomics and manufacturability rather than integrating multiple systems. - Established Use Case
The ophthalmic speculum’s use in surgery is well documented, and existing predicate devices can guide performance benchmarks, biocompatibility expectations, and clinical acceptance criteria.
What Introduces Complexity (and Cost)
Although the product’s form and function are familiar, cost and effort can still scale depending on a few overlooked details:
- Mechanical Durability Testing
The retraction mechanism (spring or screw) must be fatigue-tested over the anticipated lifecycle, particularly for reusable models. Failure modes must be identified and mitigated early. - Precision Manufacturing Requirements
For consistent performance, exacting tolerances may be required, especially in contact points that apply pressure near the eye. This could demand advanced machining, jigs, or inspection protocols. - Sterilization Validation
Because the device will be reused, cleaning validation and sterilization process qualification (e.g. steam or ethylene oxide) must be completed, even if the mechanical design is finalized. - Regulatory Documentation Burden
Although it may qualify as a Class I device, documentation for risk analysis, material compatibility, and labeling must still be assembled to support market readiness.
Strategic Takeaway
Don’t mistake simplicity for low complexity. The ophthalmic speculum avoids many high-tech challenges, but its role in delicate surgery and reusable design means tight controls are essential. Early investments in precision prototyping, sterilization compatibility, and fatigue testing can prevent delays and unlock smoother regulatory and market access later on.
TECHNOLOGICAL READINESS
Understanding where your project stands from a technology development perspective is critical for planning the path forward. This section outlines your current progress, identifies technical assets that are already in place, and maps out the next steps needed to move toward production and market entry.
Current Stage of Development
The ophthalmic speculum is currently in the concept phase, with no completed iterations or design documentation. While the basic idea or proof-of-concept has been defined, there is no physical prototype or formal risk analysis yet in place. This phase is typical for inventors who are just beginning to transition from clinical insight or personal need into product development.
At this stage, several core development tasks remain outstanding:
- Engineering drawings and CAD models have not yet been created.
- Mechanical tolerances and usability constraints have not been tested.
- No design controls, verification plans, or usability studies have been initiated.
However, beginning at the concept stage also provides flexibility, there are no legacy design decisions to overcome, and development can be approached methodically and efficiently from the ground up.
Existing Technical Assets
There are few formal technical assets yet, but the project does have one significant advantage: a granted patent. This intellectual property protects the core concept and may offer a competitive edge during commercialization. Though the patent is limited to one country, it establishes a valuable foundation for potential future filings or licensing discussions.
Additionally, you have some clinical support from a champion. This resource, while not deeply engaged yet, can help inform early-stage development choices and may be available to provide feedback on user ergonomics and surgical usability.
What’s currently missing but will become essential:
- Documented design requirements and functional specifications
- Drawings, schematics, or models for internal use and vendor quoting
- Design history files for regulatory compliance
- Clinical use case narratives to support labeling and training
What Comes Next
To mature the technology and establish a foundation for downstream work, your next steps should include:
- Technical Design Definition
Start by drafting initial design inputs, even informally. What forces must the speculum apply? How far must it open? What is the target eyelid shape and range? - Engineering Prototyping
Fabricate a basic prototype using stainless steel or polymer equivalents. This can be evaluated for hinge function, spring behavior, and user feedback. - Design Control Initiation
Begin tracking versions of the design, documenting changes, and recording rationale. This helps align early development with regulatory expectations later on. - Sterilization Compatibility Planning
Since the device is reusable, evaluate potential materials based on sterilization compatibility (e.g. steam, EO, hydrogen peroxide plasma) and durability. - IP Roadmap Refinement
Consider whether additional features, versions, or modifications might warrant follow-up patent filings, especially if international expansion is expected in the future.
Strategic Takeaway
You’re early in the development journey, but that’s not a weakness. It’s an opportunity to do things right from the start. With a patent already in place, the next step is to translate your concept into testable prototypes and design documentation. These early activities will accelerate future phases and position your product for regulatory success and commercial traction.
REGULATORY APPROVAL
Navigating the regulatory pathway is one of the most important components of medical device development. While the ophthalmic speculum is mechanically simple and lacks electronics or complex systems, its classification as a surgical instrument means it must still meet strict standards for safety, sterilization, labeling, and performance before entering the market.
FDA Classification Snapshot
- Regulation Number: 886.4350
- Product Code: HNC
- Regulation Medical Specialty: Ophthalmic
- Device Class: Class I
- Submission Pathway: 510(k) Exempt
Note: You should work with a regulatory consultant to verify the correct classification and any associated guidance documents.
Initial Risk Assessment
The ophthalmic speculum is a Class I medical device, regulated under the FDA’s category of “manual ophthalmic surgical instruments.” This classification reflects its mechanical simplicity, lack of power or electronics, and historical use in standard ophthalmic surgical procedures.
Class I devices are exempt from the 510(k) premarket notification requirement, but they are still subject to FDA General Controls, including:
- Manufacturer registration and device listing
- Labeling regulations
- Design control records (if applicable)
- Quality system compliance (21 CFR Part 820)
While 510(k) submission is not required, manufacturers must still ensure their device meets all applicable standards for safety, sterility, biocompatibility, and labeling. If the design includes atypical materials or advanced features that differ significantly from standard ophthalmic specula, additional FDA feedback or documentation may be advisable, though not mandated.
Key Regulatory Considerations
- Predicate Comparison
Even as a 510(k)-exempt device, identifying FDA-listed predicate devices is useful. It provides benchmarks for clinical use, geometry, and labeling expectations. It can also guide packaging choices and assist in discussions with procurement or clinical stakeholders. - Biocompatibility Testing
- Because the device contacts the eyelid and periorbital tissue, it must demonstrate biocompatibility under ISO 10993. Key tests include:
- Cytotoxicity
- Sensitization
- Irritation or intracutaneous reactivity
- Sterilization Validation
As a reusable surgical tool, sterilization validation remains critical. Required steps include:- Defining a validated sterilization method (typically steam autoclave)
- Demonstrating achievement of a sterility assurance level (SAL 10^-6)
- Validating durability across multiple sterilization cycles
- Labeling Requirements
Class I devices must meet FDA labeling expectations, which include:- Intended use statement (e.g., surgical retraction of eyelids)
- Clear sterilization method (if shipped sterile or reused)
- Reuse instructions (e.g., number of allowable cycles, cleaning steps)
- Manufacturer name and lot/batch traceability
International Considerations
If you plan to market the device outside the U.S., early alignment with ISO 13485 and EU MDR requirements is important. In the European Union, Class I reusable surgical instruments must undergo Notified Body review for cleaning, disinfection, and sterilization validation, even if their U.S. counterpart is 510(k)-exempt.Strategic Takeaway
With its confirmed Class I classification, the ophthalmic speculum benefits from a simplified regulatory path. However, exemption from 510(k) does not mean exemption from quality, safety, or testing expectations. Establishing robust documentation for sterilization, biocompatibility, and labeling now will protect you from future compliance issues and streamline both domestic and international market entry.MARKET POTENTIAL
The ophthalmic speculum is part of a mature category of surgical tools with consistent demand across ophthalmology, optometry, and surgical settings. While the device itself is low in complexity, its role in delicate procedures makes reliability and clinician comfort essential, creating room for thoughtful innovation and meaningful differentiation.
Market Drivers
Several key trends support ongoing demand for ophthalmic surgical instruments:
- Rising Rates of Eye Surgery
With aging populations and increasing prevalence of cataracts, glaucoma, and retinal diseases, the number of eye surgeries continues to grow globally. - Surgeon Preference for Ergonomics
Instruments that reduce hand fatigue, improve visibility, or allow for precise control are more likely to be adopted, even in low-cost categories. - Shift Toward Ambulatory Surgical Centers (ASCs)
Many ophthalmic procedures are being performed in outpatient settings, increasing demand for reliable, reusable, and portable surgical instruments. - Global Expansion of Vision Care Services
International markets, especially in Asia and Latin America, are investing in eye care infrastructure, opening up demand for surgical tools that meet basic requirements while being cost-effective and durable.
Target Segments
The target users for this product include:
- Ophthalmic Surgeons performing procedures like cataract extraction, retinal repair, or glaucoma interventions.
- Hospital and Clinic Procurement Teams seeking reliable and sterilizable surgical tools.
- Surgical Centers and ASCs with high case volume and reusable instrument preferences.
- International NGOs and Eye Care Missions that often prefer reusable, rugged instruments over disposable options for cost and environmental reasons.
Depending on your final design, there may be niche applications such as pediatric ophthalmology, oculoplastics, or micro-incision surgery that would benefit from design variations (e.g., smaller size or custom tension).
Adoption Enablers
Because the ophthalmic speculum is a familiar and widely used tool, market entry relies more on trust, ergonomics, and quality than on novelty. Enablers for adoption may include:
- Clinical Endorsements or Testimonials from surgeons who prefer the new design
- Validated Reusability and Durability Claims that reduce replacement costs
- Packaging that Supports Sterility and Transport (even if sold non-sterile)
- Clear Instructions for Cleaning and Maintenance for surgical staff
If the speculum is priced competitively and offers clear usability improvements (e.g., smoother hinge action, easier adjustment), adoption by procurement officers may follow naturally.
Revenue Considerations
As a surgical accessory rather than a capital device, this product may have a relatively low unit price but high volume potential, especially when marketed through:
- Bulk purchasing contracts
- Distributor partnerships
- OEM arrangements with surgical instrument companies
Margins may vary depending on whether the product is sold directly, through distributors, or bundled with other instruments. Being reusable supports long-term institutional relationships and opens doors for repeat sales with replacement cycles based on wear and sterilization fatigue.
Revenue Risk Factors
Several factors could affect revenue potential:
- Commoditization Pressure
Many specula are low-cost and imported, meaning you may face price sensitivity unless strong differentiators are proven. - Unclear Differentiation
If improvements aren’t perceived as valuable by end users, the device may be seen as just another version of an existing tool. - Reimbursement Disconnect
As a surgical instrument, the speculum is not reimbursed directly. Value must be shown through clinical preference and operational efficiency.
Strategic Takeaway
Though simple in form, the ophthalmic speculum has meaningful market potential, particularly if you can demonstrate ergonomic or clinical improvements. Success will rely on appealing to surgeons’ preferences and procurement needs, not just offering a cheaper option. Differentiation, user feedback, and validation will be your keys to gaining traction in this competitive but high-volume space.
DEVELOPMENT PHASES & MILESTONES
Developing a medical device, even a relatively simple surgical instrument like an ophthalmic speculum, requires structure, milestones, and clear progression through formal development phases. Below is a tailored roadmap to help you plan each stage of development, aligned with medical device best practices and FDA expectations.
Phase I: Concept Development
Goal: Define the problem, confirm market and clinical needs, and shape initial design ideas.
Key Activities:
- Gather detailed user requirements through surgeon interviews or observation
- Sketch initial design concepts
- Review existing predicate devices
- Refine unique value proposition and IP strategy
- Begin documenting preliminary design inputs
Milestone: Concept design review completed; design inputs and early sketches validated by clinical champion
Phase II: Prototype Development
Goal: Translate design concepts into functional prototypes and evaluate mechanical performance.
Key Activities:
- Develop 3D CAD models and engineering drawings
- Fabricate initial prototype using appropriate materials (e.g., stainless steel)
- Conduct bench testing on opening/closing force, hinge reliability, and overall feel
- Iterate based on clinical feedback (if feasible)
- Begin DFM (Design for Manufacturing) assessment
Milestone: Working prototype validated for basic functionality and manufacturability
Note: The regulatory cost estimates in this section include expenses associated with an optional FDA 510(k) pre-submission (Q-Sub), which, while not required, can be a valuable tool for obtaining early feedback and reducing downstream submission risk.
Phase III: Design Output & Verification
Goal: Finalize design, demonstrate that it meets design inputs, and prepare for regulatory documentation.
Key Activities:
- Complete tolerance stack-up analysis and finalize drawings
- Verify mechanical strength, usability, and durability (especially hinge/spring mechanism)
- Begin sterilization and cleaning protocol development
- Conduct initial biocompatibility testing (cytotoxicity, irritation, sensitization)
- Assemble design history file components (design outputs, verification results)
Milestone: Verified design ready for sterilization validation and regulatory submission
Performance Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Mechanical Function Test | Internal Protocol | Confirm smooth opening/closing, hinge reliability, and spring tension. |
| Dimensional Inspection | ISO 1101 / Internal Tolerances | Verify precision of component dimensions and fit across production runs. |
| Fatigue (Cycle) Testing | Custom Internal Protocol aligned with ISO 7153-1 principles | Validate mechanical durability through repeated opening/closing cycles. |
| Residual Load Verification | Internal Benchmark | Ensure force applied to eyelids is within safe and comfortable limits. |
Biological Safety Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Cytotoxicity | ISO 10993-5 | Assess if materials leach toxic substances harmful to living cells. |
| Sensitization | ISO 10993-10 | Determine potential for allergic or sensitizing reactions. |
| Irritation / Intracutaneous | ISO 10993-10 | Evaluate irritation from direct skin or mucosal contact. |
Phase IV: Validation & Regulatory Submission
Goal: Confirm the device performs as intended in a real-world context and meet all regulatory expectations.
Key Activities:
- Conduct simulated use studies and validation of sterilization and reprocessing instructions
- Finalize all labeling, instructions for use (IFU), and packaging requirements
- Document conformance with FDA General Controls (and 510(k) exemption if applicable)
- Submit establishment registration and device listing to FDA
- Prepare for international expansion if applicable (e.g., CE Mark)
Milestone: Validation report completed; product registered/listed with FDA
Sterilization & Reprocessing Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Steam Sterilization Validation | ISO 17665 / AAMI ST79 | Confirm sterility assurance level (SAL 10^-6) is achieved with selected method. |
| Cleaning Effectiveness Evaluation | AAMI TIR30 / ISO 15883 | Demonstrate effective cleaning between uses. |
| Residual Contaminant Assessment | ISO 11737-1, USP <1227> | Check for chemical, biological, or particulate residues post-cleaning. |
| Reuse Lifecycle Durability Study | Internal Protocol | Evaluate mechanical and material integrity across repeated sterilization cycles. |
Usability Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Formative Usability Review | FDA Guidance on Human Factors | Collect clinician feedback on ergonomics, feel, and ease of use. |
| Simulated Use Testing | Internal Protocol / IEC 62366-1 | Observe actual use in simulated surgery to identify safety or workflow gaps. |
Packaging and Environmental Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Packaging Integrity Testing | ASTM F88 / ASTM F1929 | Ensure packaging seals are strong and leak-free. |
| Transportation Simulation Testing | ASTM D4169 | Assess packaging and product durability during shipping and handling. |
Phase V: Full-Scale Production & Launch
Goal: Transition from validated prototype to production and begin marketing/sales activities.
Key Activities:
- Qualify manufacturing processes and vendors
- Finalize QC inspection protocols
- Order initial production run
- Train internal or distributor sales teams
- Launch website, marketing materials, and KOL engagement
Milestone: Product launched commercially and in active distribution
Each phase has its own technical and business challenges, but the biggest delays typically happen when design, testing, or regulatory planning are rushed or skipped early on. By following a phased model and closing out each milestone thoroughly, you set yourself up for a smoother regulatory path, stronger manufacturing handoff, and faster market entry.
Note: The tests above are provided as illustrative examples to reflect the expected level of complexity and rigor required during the development of the product. Final tests, plans and protocols may vary based on the finalized design, risk assessment, and regulatory strategy.
RESOURCE ALLOCATION & TEAM INVOLVEMENT
Developing even a simple, mechanical medical device requires coordination across several functional areas. While your ophthalmic speculum doesn’t involve electronics or complex systems, success will still rely on having the right contributors at each stage, from concept refinement through to launch.
Core Functional Roles Required
Here are the essential roles to support a smooth development pathway for your device:
- Mechanical Engineer
To lead CAD modeling, tolerance analysis, and design for manufacturing (DFM). - Industrial Designer (optional)
To support ergonomic improvements, especially if the device is intended to compete on surgeon comfort. - Clinical Advisor
To provide feedback on usability, retraction force, and compatibility with surgical workflows. - Quality & Regulatory Specialist
To prepare documentation, interpret FDA regulations, and manage labeling, sterilization validation, and submission requirements. - Manufacturing Partner or Machinist
To fabricate prototypes and later scale production with appropriate tolerances and material handling.
If your team is small, some roles may be combined, but all responsibilities must be accounted for.
Specialty Support Needs
Although no software or electronics are involved, there are specialty areas that require external or expert support:
- Biocompatibility Consultant or Testing Lab
For interpreting ISO 10993 requirements and running irritation, sensitization, and cytotoxicity tests. - Sterilization Validation Vendor
To guide and execute sterilization cycle validation and reprocessing simulations. - Patent Attorney (if IP expansion planned)
To evaluate derivative ideas and assist with foreign filings.
You may also benefit from an FDA regulatory consultant if planning to expand to international markets or unfamiliar with Class I device requirements.
| Phase | Contributors |
| Concept | Inventor, Clinical Advisor |
| Prototype | Mechanical Engineer, Clinical Advisor |
| Testing & Validation | Mechanical Engineer, Quality Specialist, Testing Vendors |
| FDA Submission | Regulatory Specialist, Quality Manager |
| Production & Launch | Manufacturing Partner, Mechanical Engineer, Sales Team |
As the project grows, these roles may expand or shift based on budget and market strategy.
Strategic Takeaway
Even for low-tech devices, a well-rounded team is essential. Identifying contributors early and assigning clear responsibilities across development phases reduces the risk of gaps, delays, or regulatory setbacks. Think of your resource map as a checklist for forward progress; each contributor plays a key role in transforming your idea into a commercial product.
RISK MITIGATION STRATEGIES
Every medical device project, regardless of its complexity, faces technical, regulatory, and operational risks. For a surgical tool like the ophthalmic speculum, these risks may not involve electronics or software, but they still demand proactive planning and testing. Below is a breakdown of the key risk categories relevant to your project and strategies to mitigate them.
Usability Risks
- Risks
- Excessive retraction force could cause patient discomfort or tissue trauma.
- Difficult-to-operate hinge or locking mechanisms may distract surgeons during procedures.
- Poor ergonomics could lead to hand fatigue or increased setup time.
- Mitigation Strategies
- Involve clinical advisors early in prototype reviews to provide real-time feedback.
- Simulate typical surgical workflows to identify friction points.
- Explore adjustable models or offer multiple size options to improve surgeon fit and preference.
Performance Risks
- Risks
- Mechanical failure under repeated use (e.g., spring fatigue, loose hinges).
- Inconsistent force application or alignment, especially in low-cost manufacturing batches.
- Inadequate durability through repeated sterilization cycles.
- Mitigation Strategies
- Conduct mechanical fatigue testing on the retraction mechanism.
- Set tolerance thresholds during DFM to ensure reliable batch consistency.
- Validate material selection for high strength and corrosion resistance.
Mechanical Safety Risks
- Risks
- Sharp edges or burrs could cause accidental cuts during handling or use.
- Binding or pinching hazards during device operation.
- Device deformation due to high clamping force or thermal cycles.
- Mitigation Strategies
- Apply stringent surface finish criteria in design documentation.
- Include a mechanical safety inspection in the final QA protocol.
- Use controlled thermal exposure tests to confirm shape retention post-sterilization.
Regulatory Risks
- Risks
- Misinterpreting the scope of 510(k) exemption and failing to meet all Class I requirements.
- Overlooking labeling requirements for cleaning, reuse, or instructions for use (IFU).
- Incomplete or missing documentation for biocompatibility or sterilization validation, despite exemption from premarket notification.
- Mitigation Strategies
- Confirm and document FDA Class I classification and exemption status early in the project.
- Draft and review compliant labeling, IFU, and reprocessing instructions during the design phase.
- Engage test labs or consultants to outline ISO 10993 biological safety and sterilization requirements, ensuring all supporting documentation is prepared for inspection or international submissions.
- Risks
- Delays in sourcing custom components or materials suitable for sterilization.
- Vendor variability affecting fit and finish of critical mechanical parts.
- Long lead times for small production runs or specialty finishing processes.
- Mitigation Strategies
- Select vendors experienced in surgical-grade instrument manufacturing.
- Qualify at least one backup supplier for critical components.
- Use standard part geometries where possible to reduce tooling dependency.
Strategic Takeaway
While your ophthalmic speculum may seem mechanically simple, it still carries meaningful risks, especially in terms of usability, fatigue resistance, and regulatory assumptions. Risk mitigation is most effective when it begins early, builds into each phase of development, and includes both lab testing and real-world clinician input.INVESTMENT & FINANCIAL OUTLOOK
Bringing a Class I reusable surgical instrument like the ophthalmic speculum to market can be more cost-effective than complex electronic devices, but that doesn’t mean the path is inexpensive. Development, validation, and regulatory compliance still require strategic investments, particularly if long-term success and international scalability are part of your vision.
Primary Cost Drivers
For this device, the most significant cost contributors will include:
- Prototyping & Iteration
While not electronics-heavy, multiple prototypes may be needed to optimize mechanical performance, spring strength, and ergonomics. - Sterilization Validation
As a reusable Class I device, sterilization validation (e.g., steam autoclave) and cleaning effectiveness studies must still be conducted to support labeling and instructions for use. - Biocompatibility Testing
ISO 10993 testing, particularly for cytotoxicity, sensitization, and irritation, is required due to direct tissue contact, even in the absence of a 510(k) submission. - Tooling for Manufacturing
Even minor design changes can trigger additional tooling or fixture costs during the transition from prototype to production. - Quality & Regulatory Support
Although 510(k) submission is not required, expert support is still essential to ensure labeling, sterilization instructions, biocompatibility documentation, and general FDA compliance are properly addressed.
Budgeting Tips for Early Inventors
- Bundle Activities When Possible
For example, combine mechanical testing with early usability evaluations to reduce rework. - Plan for Reuse Validation Early
Since this is a reusable instrument, build in testing and documentation for multiple sterilization cycles upfront. - Avoid Over-Engineering
Focus on performance improvements that matter clinically. Custom features that don't enhance function can inflate cost without improving adoption. - Leverage Predicate Devices
Where appropriate, reference existing biocompatibility and material usage data to reduce testing costs.
Funding Strategy Considerations
Given its scope and complexity, this device may be well-suited for:
- Self-funding or Angel Investors
Especially in early phases where IP and clinical traction can be demonstrated with relatively low capital. - Grants or Non-dilutive Funding
Organizations supporting vision care and global health (e.g., USAID, NIH NEI, or NGOs) may support reusable ophthalmic tools. - Strategic Partnerships
Teaming up with established surgical tool manufacturers or distributors could provide a path to co-development or white labeling.
If the goal is to scale manufacturing internationally, additional funding rounds may be needed to expand testing scope and quality system infrastructure.
Revenue Potential Considerations
Revenue will depend on:
- Volume vs. Margin Tradeoffs
A reusable tool like this often sells in volume to clinics or surgical centers, where price sensitivity is high, but so is repeat ordering. - Clinical Differentiation
The more clearly the product improves surgeon comfort or performance, the more premium pricing can be justified. - Bundling Opportunities
Packaging the speculum with other surgical tools (or licensing it to OEMs) can accelerate revenue without building a full distribution model in-house.
Financial Risk Mitigation
- Pilot Production Before Scaling
Run a limited batch to identify manufacturing issues early. - Confirm Regulatory Pathway Before Spending on Testing
Make sure the Class I designation and exemption apply before proceeding with costly validation work. - Protect IP Early
The granted patent is a strength, ensure it’s enforced, and explore international filing if expansion is on the horizon.
Strategic Takeaway
The ophthalmic speculum presents a compelling case for controlled, capital-efficient development. By focusing on key testing, careful vendor selection, and thoughtful partnerships, you can minimize financial risk while building a device that meets clinical needs and supports sustainable revenue.
Your Complimentary Q&A
Have questions about the report?
Book a 15-minute call to clarify insights or prioritize next steps.
Understanding Vendor Tiers and Impact on Project Cost and Time
Tier 1: Higher costs associated with comprehensive services complete system development, advanced technology, and the ability to manage complex projects. Design services may have shorter lead times due to ability to build a larger team however the scale of operations and the complexity of the more comprehensive supply chain may slow certain processes.
Tier 2: Their cost and Time may vary based on their specialization allowing for efficient production of specific components, potentially leading to shorter lead times for those items. However, since they do not provide complete systems, the overall integration into larger assemblies may require additional coordination, potentially affecting timelines.
Tier 3: Lower costs due to specialization in specific components or materials or limited staffing resources requiring additional coordination with other suppliers. This may slow the development time from both a design and supply chain perspective.
Considerations
- Despite higher costs and longer lead times, Tier 1 suppliers may be more suitable for complex projects requiring integrated solutions.
- For projects with budget constraints, engaging multiple Tier 3 suppliers could be more cost-effective, but may require more intensive project management.
- Working with Tier 3 suppliers entails coordinating a robust supply chain to ensure timely delivery and quality assurance.
The choice between Tier 1 and Tier 3 suppliers involves trade-offs between cost, time, and supply chain management complexity. Careful evaluation of project requirements and resources is essential for making an informed decision.
Disclaimers & Limitations
- Generalizations: This report provides a high-level overview based on standard assumptions and does not account for unique device characteristics. Actual costs, timelines, and risks may vary significantly depending on the device's design, use case, and target market.
- Assumptions of Device Class and Use: Assumptions were made regarding the device's classification and intended use. These assumptions can impact regulatory requirements, costs, and timelines. Specific regulatory pathways, for instance, may differ based on the device's risk classification and market entry strategy.
- Market and Regulatory Dynamics: Regulatory requirements and market conditions are subject to change. The report's cost and timeline estimates may be affected by evolving regulatory landscapes, standards, or unforeseen market dynamics, which could delay approval or require additional testing.
- Risk Assessment Limitations: Risk levels and mitigation strategies are based on general device categories and may not fully address specific technical or operational risks unique to the product. Thorough risk assessments should be tailored to the device's complexity, materials, and usage.
- Development Phases and Milestones: The development phases outlined here follow a typical medical device development pathway, but real-world project phases may overlap or require iteration due to unforeseen challenges or design changes.
- Cost and Timeline Variability: The cost and timeline estimates are based on standard industry benchmarks but do not account for project-specific adjustments. Factors like unexpected technical challenges, prototype iterations, or regulatory re-submissions can significantly impact final costs and schedules.
- Reliance on Industry Standards: The report relies on common industry standards for development and testing. However, additional standards specific to certain device features or regions may apply, affecting compliance requirements and associated timelines.
- Testing and Validation Scope: Testing and validation requirements are generalized. Devices with novel materials, complex electronics, or unique features may require additional, specialized tests, potentially extending both cost and duration.
READY FOR EVEN MORE INSIGHTS?
Unlock for $29.95- Regulatory pathway and market opportunity
- Milestone roadmap with phase activities
- Team and resource playbook
- Risk factors and mitigation strategies
- Financial planning and commercialization outlook
UNLOCK NOW
- Development cost and timeline benchmarks
- Complexity insights shaping risk and effort
- Technology readiness snapshot
.png?width=4200&height=441&name=Zewski_Report%20Logo%20(Shirts).png)