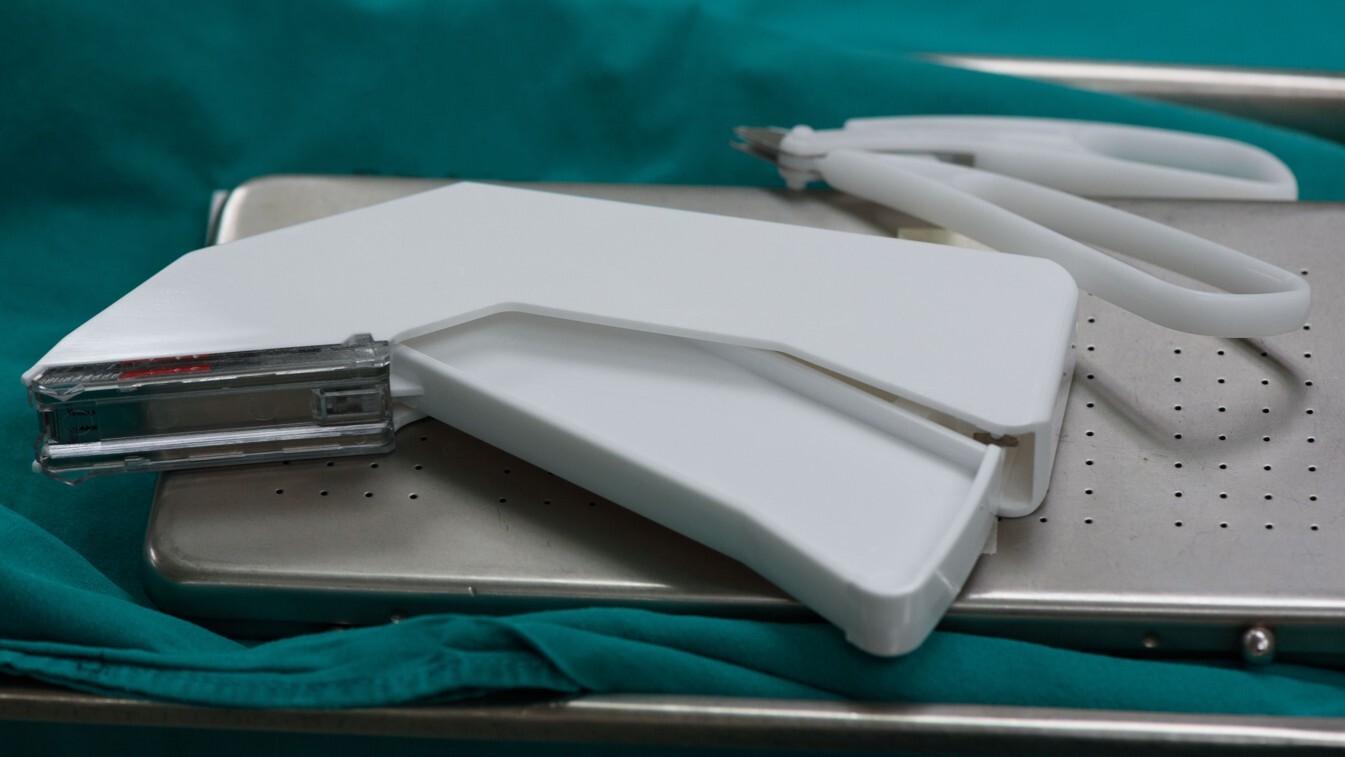
Image is for illustrative purposes only.
Surgical Skin Stapler, or Similar
GETTING STARTED
This report is a roadmap preview for a Surgical Skin Stapler – not a custom plan. It’s framed as if starting from scratch, highlighting the typical development steps, costs, and hurdles common to devices in this category. Use it to find patterns that apply to your project even if features differ.
As you read:
Look for parallels with your own concept.
Pay attention to phase transitions – that’s where costs and timelines often shift.
Use the benchmarks as reference points, not exact budgets or schedules.
Share it with partners or investors to set realistic expectations from the start.
The aim is to show likely complexities early so you can plan with confidence.
DEVICE OVERVIEW
The Surgical Skin Stapler is a handheld, mechanically operated medical device designed to close wounds by delivering surgical staples to the outer layers of the skin. This device is used primarily in surgical settings where quick and secure closure is needed, especially in procedures requiring reduced operating time and minimal tissue trauma.
Unlike sutures, which require individual placement, surgical staplers deploy multiple staples in a uniform pattern with a single motion, providing consistent approximation of the skin edges. This not only improves procedural efficiency but also supports better cosmetic outcomes in many cases.
This stapler is envisioned as a medium-sized, reusable tool composed of a combination of materials, likely including stainless steel for strength and sterilizability, paired with medical-grade plastics for ergonomic handling. Notably, the design excludes any electrical or electronic components, relying instead on complex mechanical linkages and manual actuation to drive the staples into the skin.
The product is classified by the FDA as a surgical stapler for external use, a prescription device intended for physician use in hospitals, operating rooms, or outpatient surgical centers. Although external-use staplers are typically lower-risk than internal surgical staplers, they still require careful validation to ensure reliability, user safety, and clinical efficacy.
Because this stapler is designed to be reusable with extensive cleaning, particular attention must be paid to its material interfaces, hinge mechanisms, and disassembly protocols. Ensuring reliable sterilization between uses will be a core part of the design-for-reprocessing strategy.
Strategic Takeaway
The Surgical Skin Stapler offers an efficient and standardized approach to skin closure in surgical procedures. Its mechanical, handheld design eliminates the need for power or electronics while demanding careful mechanical engineering and material selection to ensure safe reuse. Understanding its role in the clinical workflow is essential to shaping both development and regulatory strategies moving forward.
FEASIBILITY
Understanding Your Feasibility Score
The Feasibility Score bar provides an assessment of your project’s path to market, with higher values indicating lower complexity and fewer anticipated obstacles.
- 0 - 39 (Low Feasibility): This range suggests that the project may face significant challenges due to high complexity or extensive requirements. Additional planning, resources, or risk mitigation strategies will be necessary.
- 40 - 74 (Moderate Feasibility): Projects within this range indicate a moderate path to market. While the overall complexity is manageable, some areas may require refinement or further development to ensure project stability and success.
- 75+ (High Feasibility): A score in this range indicates a relatively straightforward path to market, with low complexity and minimal additional work expected. This project is well-positioned to progress smoothly.
The Feasibility Score is a general guide, not an absolute measure of project success. We recommend using this score as part of a broader assessment and considering additional expert guidance for a comprehensive evaluation.
PROJECT OVERVIEW
The development of this Surgical Skin Stapler sits at the very beginning of the medical device innovation journey. With a concept or proof-of-concept in hand, and no iterations or formal documentation completed, the project represents a classic early-stage effort, one filled with potential, but also requiring strategic planning and staged execution.
Early-Stage, High-Potential Foundation
The presence of a granted patent, even if limited to a single country, is a promising foundation. Intellectual property protection this early in development suggests a clear idea with unique features, something slightly different from what's already on the market. That uniqueness will need to be further defined as the team moves toward positioning the stapler among predicate devices for regulatory clearance.
From a clinical standpoint, the device benefits from clinical support, even if that champion is not fully embedded in the development effort. Having a clinician who believes in the idea can be a critical asset for refining real-world use cases, identifying unmet needs, and eventually facilitating validation through studies or pilot use.
What Makes This Project Unique
While the device is fundamentally mechanical and shares similarities with other skin staplers, a few characteristics set this project apart:
- Reusable design, which places it in contrast with the many single-use disposable staplers in the market.
- Complex mechanical parts, requiring detailed engineering to ensure consistent function after repeated cycles of use and sterilization.
- Off-the-shelf component usage, which, if feasible, could dramatically streamline sourcing and production ramp-up.
These differentiators are important not only for engineering but also for how the product might fit into healthcare systems under cost constraints or sustainability initiatives.
What Lies Ahead
Because the project is still in the concept phase, the next steps involve translating the idea into reality. This includes:
- Developing initial sketches and CAD models
- Defining functional requirements and performance criteria
- Exploring materials that balance durability with sterilizability
- Mapping the early design control elements required for Class I medical devices
As no design-for-manufacturing (DFM) activities have yet occurred, the team will need to move carefully into early prototyping while also establishing critical documentation for future regulatory alignment.
Strategic Takeaway
This Surgical Skin Stapler project represents a well-positioned but early-stage effort with a unique combination of mechanical complexity, clinical support, and IP protection. The next stretch of work will focus on converting a protected idea into a documented, tested, and manufacturable medical device, with early attention to reuse, performance, and market fit.
COST & TIME ESTIMATES
DEVELOPMENT COMPLEXITY
Developing a surgical skin stapler, especially one that is reusable and mechanically actuated, requires thoughtful planning across engineering, manufacturing, and regulatory domains. While it avoids the complications of electronics and software, the device introduces other forms of complexity, particularly around its mechanical design and reusability.
Primary Drivers of Complexity
Several elements contribute to the technical and logistical complexity of this product:
- Complex Mechanical Components
The stapler will require precisely engineered mechanisms to ensure repeatable staple delivery with proper depth and alignment. Cam arms, springs, triggers, and staple-feed tracks must operate smoothly together, even after multiple uses and cleanings. Achieving consistency without powered assistance places high demands on mechanical tolerancing. - Reusable Design with Extensive Cleaning
Reusability introduces an entirely separate design challenge: all components must survive repeated sterilization cycles (typically high-heat autoclaving or chemical treatment) without degradation. Hinges, small moving parts, and multi-material joints must be designed to avoid trap points for biological debris and allow for full disassembly or validated cleaning protocols. - Superficial Invasiveness
Although the device only interacts with skin and not deeper tissues, it is still classified as superficially invasive, which means biocompatibility, performance, and safety verification testing are essential.
What Simplifies Development
Despite its challenges, a few factors help streamline the process:
- No Electronics or Software
Without embedded electronics, firmware, or displays, the device avoids the extensive documentation and testing required under IEC 62304 (software lifecycle), EMC compliance, and electrical safety standards. This reduces time, cost, and potential regulatory hurdles. - Simple Supply Chain (Mostly Off-the-Shelf Components)
The reliance on commonly available components and materials can reduce lead times and simplify sourcing. Early prototypes can often be built without full tooling, and later-stage builds may benefit from lower per-unit costs due to bulk availability of standardized parts. - No Customization Requirements
Since the product is not tailored to individual patients or procedures, the design scope remains focused. This allows for clearer specifications and fewer validation scenarios.
What Introduces Complexity (and Cost)
Even without electronics, cost and complexity can still escalate in these areas:
- High-Precision Manufacturing Requirements
Reliable staple deployment depends on fine-tuned dimensions, which often translates into higher-precision machining, especially for the cartridge track, trigger mechanism, and staple-forming anvil. - Material Compatibility for Sterilization
Selecting materials that are both durable and biocompatible while withstanding autoclaving is a non-trivial task. Additionally, multiple materials in one device must be bonded or joined in ways that do not degrade over time or compromise cleaning. - Testing Burden for Reuse Claims
Reusable devices must undergo extensive cleaning validation, simulated use cycles, and performance repeatability testing. This testing can be both time-intensive and expensive, even for Class I products.
Strategic Takeaway
While the Surgical Skin Stapler benefits from a mechanically simple (non-electronic) design and accessible supply chain, its reusability, mechanical complexity, and safety-critical function introduce notable challenges. Success will hinge on precision engineering, durable material choices, and rigorous performance validation to ensure safe, repeatable operation across its expected lifespan.
TECHNOLOGICAL READINESS
Understanding where the surgical stapler currently stands in its development lifecycle is key to planning next steps. While the concept is promising and protected by a patent, it remains early in its execution. This section outlines the current state and the progression needed to advance the technology toward production readiness.
Current Stage of Development
Based on the provided inputs, the device is currently in the concept or proof-of-concept phase. There are no documented iterations, no design control documentation initiated, and no formal prototypes yet created. While this is typical for early-stage medtech innovations, it means that nearly all of the technical groundwork, including functional definition, CAD development, and usability considerations, still lies ahead.
Key characteristics of the current stage:
- No prior iterations to build upon or learn from
- No documented requirements or specifications
- No physical prototypes constructed
- No DFM (Design for Manufacturing) effort initiated
While the project is just beginning, the presence of a granted patent suggests the core design concept has already been articulated clearly enough to meet novelty and non-obviousness criteria, an encouraging sign for future technical development.
Existing Technical Assets
Although technical documentation is lacking, one key asset exists:
-
A granted patent covering the core innovation, protected in one jurisdiction.
This intellectual property can serve as both a design guide and a marketing differentiator, especially when seeking investment or identifying predicate devices for regulatory strategy. However, the lack of physical models, stress analysis, user feedback, or testing results places the project in a pre-engineering state.
What Comes Next
To transition from concept to feasibility and then toward commercialization, several core activities should be prioritized:
- Initial Design Documentation
- Define the device's functional requirements (e.g., staple depth, actuation force, cleaning process).
- Draft initial CAD models or hand sketches to visualize geometry and moving parts.
- Prototyping and Design Iteration
- Construct early mechanical prototypes using 3D printing or machined components.
- Conduct simulated use or bench tests to evaluate the core mechanism.
- Material Feasibility Assessment
- Identify materials that meet biocompatibility and sterilization standards.
- Conduct limited testing for wear, corrosion, and thermal resistance if possible.
- Initiate Design Controls
- Begin compiling traceable documentation (design inputs, risk analysis, verification plan).
- This is especially critical to ensure future compliance with regulatory expectations, even for Class I devices.
- Evaluate Sterilization Compatibility
- Plan ahead for sterilization validation. Reusable devices must survive repeated exposure to high-temperature or chemical sterilants without degradation.
- Clinical Use Simulation and Feedback
- Involve your clinical champion in evaluating early models for ergonomics, usability, and procedural workflow fit.
Strategic Takeaway
Technologically, this surgical stapler is in its earliest actionable stage. Moving forward will require establishing technical documentation, building and testing mechanical prototypes, and validating the concept through clinician feedback and performance simulations. Early investment in design controls, even for a Class I device, will pave the way for smoother regulatory and manufacturing paths later on.
REGULATORY APPROVAL
Navigating the FDA regulatory process is essential, even for Class I devices like this surgical skin stapler. While Class I products typically follow a more streamlined pathway and may be exempt from premarket notification (510(k)), they are not exempt from meeting general controls, which include labeling requirements, good manufacturing practices, and compliance with applicable standards such as biocompatibility and reprocessing validation for reusable devices.
FDA Classification Snapshot
- Regulation Number: 878.4740
- Product Code: QQS
- Regulation Medical Specialty: General Hospital
- Device Class: Class I
- Submission Pathway: 510(k) Exempt
Note: You should work with a regulatory consultant to verify the correct classification and any associated guidance documents.
Although skin staplers are widely used and well understood, the reusable nature of this particular design requires close attention to applicable FDA expectations, particularly around safety, performance consistency, and cleanliness after reprocessing.
Key Regulatory Considerations
- Reusable Device Reprocessing Validation
Reusable Class I devices must comply with FDA guidance on reprocessing and cleaning validation, including:- Demonstration that the device can be effectively cleaned and sterilized for safe reuse.
- Documentation that cleaning instructions provided in the Instructions for Use (IFU) are validated and repeatable in real-world settings.
- Material compatibility with sterilization methods (e.g., autoclave, chemical disinfectants) must be demonstrated.
- Biocompatibility Testing
Although the device contacts only intact skin, it still falls under superficial invasive classification. Therefore, per ISO 10993-1, the following biocompatibility evaluations may apply:- Cytotoxicity
- Sensitization
- Irritation or Intracutaneous Reactivity
- Labeling and Instructions for Use (IFU)
Even without a 510(k), FDA expects:- Clear and validated IFUs including usage, cleaning, and sterilization steps.
- Appropriate warnings, contraindications, and storage instructions.
- UDI compliance and inclusion of required symbols per FDA and international labeling standards.
- Design Controls and Risk Management
Design controls under 21 CFR Part 820 are mandatory, even for exempt Class I devices. This includes:- Design input/output traceability
- Risk analysis (e.g., FMEA)
- Verification activities and test plans
- Final design reviews and approvals
International Considerations
If expansion to other markets (e.g., EU, Canada, Australia) is anticipated, additional standards will apply:
- EU MDR Classification for reusable surgical instruments
- CE Marking requires GSPR compliance and a technical file
- Local language translations, IFU customization, and notified body reviews may be needed
Even though this may not be an immediate focus, early planning for international readiness can simplify future market expansion.
Strategic Takeaway
Although this surgical stapler is classified as a Class I device and likely qualifies for exemption from 510(k), it is still subject to important regulatory requirements, especially due to its reusable design. Cleaning validation, biocompatibility testing, and clear IFUs will be pivotal to a compliant and commercially viable product. Early integration of regulatory strategy into your development process will reduce costly delays and support a smoother path to market.
MARKET POTENTIAL
Surgical skin staplers represent a mature product category, but this also means there's an established demand and clear usage pattern across surgical specialties. The key to successful market entry for a new device, especially one that's only slightly unique, lies in offering incremental value while aligning with cost-conscious and efficiency-driven healthcare environments.
Market Drivers
Several trends support continued demand for surgical staplers:
- High volume of surgical procedures globally, including emergency trauma care, general surgery, and outpatient skin closures.
- Focus on speed and consistency, especially in high-throughput operating rooms, where staplers can reduce closure time compared to sutures.
- Staffing shortages, which increase demand for intuitive, easy-to-use tools that reduce variability between users.
These forces favor handheld, ergonomic, and reusable solutions, especially those that reduce waste or lower long-term procedural costs.
Target Segments
This stapler’s reusable format and manual operation position it well for:
- Hospitals with centralized sterilization departments, where reusable instruments can be efficiently processed and tracked.
- Military and field surgery applications, where battery-free, rugged, and reusable tools are preferred.
- Outpatient surgery centers focused on recurring procedures (e.g., dermatologic surgery, minor trauma repair).
- Global health markets, particularly in regions where single-use devices are cost-prohibitive or logistically difficult to replace.
A narrow product scope with a competitive price point could allow penetration into both high-resource and under-resourced healthcare systems.
Adoption Enablers
Factors that will influence adoption include:
- Clinical comfort with staples, which are widely accepted and require minimal retraining.
- Durability and ease of cleaning, which help facilities justify the cost of reusability.
- Consistent staple formation and release force, ensuring reliability across uses and users.
- Availability of compatible refill cartridges (if applicable), or an integrated staple cartridge with clear reload guidance.
Even minor ergonomic improvements, such as easier grip, reduced trigger force, or one-handed actuation, could differentiate the product in a crowded market.
Revenue Considerations
Revenue potential hinges on two critical factors:
- Initial device pricing
Reusability allows a higher upfront price, but value must be proven over time. - Staple refill model
If staples are proprietary or sold separately, a recurring revenue stream may be possible.
Bundled pricing, value-based contracting (e.g., price per procedure), or reprocessing kits could also enhance the business model, especially if the device performs well in durability testing.
Revenue Risk Factors
- Commoditization
The stapler market includes many low-cost competitors. Hospitals may be reluctant to switch unless a clear benefit is demonstrated. - Cleaning/validation burden
Reusable tools must meet high standards for infection control. If your stapler is perceived as difficult to clean or validate, adoption may stall. - Procurement preferences
Many institutions have purchasing contracts for disposable surgical supplies. Breaking into those systems can be challenging without a compelling economic argument.
Strategic Takeaway
While the surgical stapler market is mature, the right combination of durability, ease of reprocessing, and mechanical reliability can open a viable path to adoption, especially in high-volume or cost-sensitive settings. Positioning the stapler as a sustainable, high-performance alternative to disposables could unlock niche markets and recurring revenue streams with minimal workflow disruption.
DEVELOPMENT PHASES & MILESTONES
To guide the Surgical Skin Stapler from concept to commercialization, development should follow a phased approach, each with clear goals, deliverables, and decision points. These stages ensure the device is not only functional and manufacturable, but also aligned with regulatory and market requirements.
Phase I: Concept Development
Goal: Translate the core idea into a foundational product architecture with documented design intent.
Key Activities:
- Define user needs and functional requirements
- Initiate CAD modeling and early hand sketches
- Identify key mechanical components and motion paths
- Outline cleaning and sterilization strategy
- Conduct early competitive and market analysis
- Align with clinical champion to refine use cases
Milestone: Preliminary design concept documented and reviewed with stakeholder input.
Phase II: Prototype Development
Goal: Build and test early prototypes to validate core mechanical function and explore feasibility of reuse.
Key Activities:
- Fabricate alpha and beta prototypes (e.g., 3D printed or machined)
- Conduct mechanical testing of trigger and staple deployment
- Perform limited-use cycle testing for reusability assumptions
- Evaluate disassembly/reassembly for cleaning procedures
- Begin material selection focused on sterilization durability
- Update risk analysis and design inputs
Milestone: Functional prototype demonstrates reliable staple delivery and cleaning pathway feasibility.
Note: The regulatory cost estimates in this section include expenses associated with an optional FDA 510(k) pre-submission (Q-Sub), which, while not required, can be a valuable tool for obtaining early feedback and reducing downstream submission risk.
Phase III: Design Output & Verification
Goal: Finalize the design and verify that all engineering and risk requirements are met through structured testing.
Key Activities:
- Lock final geometry and mechanism tolerances
- Conduct verification testing (e.g., cycle testing, mechanical force, staple penetration)
- Perform biocompatibility testing (cytotoxicity, sensitization, irritation)
- Validate cleaning and sterilization methods for reuse
- Create draft labeling, instructions for use, and risk documentation
- Finalize bill of materials and design files
Milestone: Design Verification Report completed with testing data supporting performance and safety claims.
Performance Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Staple Formation Consistency | Internal Protocol | Confirm each staple forms uniformly and with adequate skin approximation. |
| Actuation Force Testing | Internal Protocol | Validate trigger force is within ergonomic range across use cycles. |
| Mechanical Endurance (Cycle Testing) | Internal Protocol (based on ISO 13485 / AAMI TIR38 guidance) | Simulate extended use and reprocessing cycles (e.g., 100+ actuations). |
| Staple Misfire / Jam Frequency | Internal Protocol | Track and limit failure modes during testing cycles. |
Biological Safety Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Cytotoxicity | ISO 10993-5 | Ensure materials do not induce cell toxicity. |
| Sensitization | ISO 10993-10 | Evaluate potential for allergic response on skin. |
| Irritation / Intracutaneous | ISO 10993-10 | Confirm no adverse skin irritation or reactivity occurs. |
Phase IV: Validation & Regulatory Submission
Goal: Confirm that the final design meets user needs and regulatory requirements; complete all premarket documentation.
Key Activities:
- Validate clinical usability through simulated-use studies or expert feedback
- Finalize sterilization and cleaning validation data
- Assemble Design History File (DHF)
- Prepare labeling, IFU, and Unique Device Identifier (UDI) if required
- Confirm Class I Exempt status or prepare 510(k) if exemption doesn’t apply
- Submit documentation for market clearance (if needed)
Milestone: Design validated, all documentation complete, and ready for registration and commercial release.
Cleaning, Sterilization & Reuse Validation Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Cleaning Validation (Manual/Automated) | AAMI TIR30 / FDA Reprocessing Guidance | Demonstrate cleaning effectiveness between uses. |
| Simulated Use + Reprocessing Cycles | AAMI ST98 / ASTM F3127 | Confirm function and appearance remain intact after sterilization cycles. |
| Material Compatibility with Sterilization | ASTM F86 / ISO 17665 (steam) or ISO 11135 (EtO) | Ensure materials don’t degrade with sterilant exposure. |
| Dry Time / Residual Moisture Assessment | Internal SOP | Confirm drying is complete post-cleaning to avoid microbial growth risk. |
Packaging and Environmental Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Packaging Integrity Testing | ASTM F1929 / ASTM F2096 | Ensure packaging remains intact through shipping and handling. |
| Accelerated Aging (if applicable) | ASTM F1980 | Estimate shelf life of device and packaging system. |
Usability & Human Factors Testing Matrix
| Test Name | Standard / Reference | Purpose |
| Formative Usability Evaluation | IEC 62366-1 (informal) | Assess comfort, hand fit, and feedback during prototype evaluation. |
| Cleaning Procedure Usability |
Internal IFU Simulation | Validate ease of disassembly and adherence to cleaning instructions. |
Phase V: Full-Scale Production & Launch
Goal: Transition from prototype to full-scale manufacturing with quality controls and production workflows established.
Key Activities:
- Finalize production tooling and quality inspection procedures
- Establish sterilization, cleaning, and packaging protocols
- Implement traceability and UDI systems
- Train production staff and/or contract manufacturer
- Conduct limited launch or pilot distribution
- Collect post-market feedback for future revisions
Milestone: Device released to market with quality systems in place and early production data collected.
Each phase has its own technical and business challenges, but the biggest delays typically happen when design, testing, or regulatory planning are rushed or skipped early on. By following a phased model and closing out each milestone thoroughly, you set yourself up for a smoother regulatory path, stronger manufacturing handoff, and faster market entry.
Note: The tests above are provided as illustrative examples to reflect the expected level of complexity and rigor required during the development of the product. Final tests, plans and protocols may vary based on the finalized design, risk assessment, and regulatory strategy.
RESOURCE ALLOCATION & TEAM INVOLVEMENT
Bringing a reusable surgical skin stapler to market requires coordinated input from specialists across engineering, clinical, and regulatory domains. The team doesn't need to be large, but it must be cross-functional, technically proficient, and strategically aligned with the project’s phased development model.
Core Functional Roles Required
To support this device’s mechanical complexity and reusability profile, the following core roles should be engaged:
- Mechanical Engineer
Designs and iterates the staple deployment mechanism, defines tolerances, and ensures repeatable performance across use cycles. - Design for Reuse Specialist or Sterilization Consultant
Advises on materials, component separability, and cleaning validation. Ensures compliance with FDA and ISO sterilization guidance for reusable instruments. - Industrial Designer
Optimizes ergonomics, aesthetics, and user experience, especially for one-handed use and staple reload scenarios. - Regulatory Affairs Expert
Interprets FDA expectations for reusable Class I devices, supports design controls documentation, and ensures compliance with labeling, IFU, and UDI requirements. - Clinical Advisor
Provides hands-on feedback during prototype evaluations and validates clinical usability assumptions for different procedural contexts. - Prototyping Technician or Vendor
Rapidly fabricates mechanical builds for in-house or clinician testing.
Specialty Support Needs
While not always full-time roles, these additional contributors can accelerate development and ensure long-term scalability:
- Materials Scientist (for biocompatibility and sterilization compatibility)
- Quality Assurance Specialist (especially during Phase III & IV)
- Manufacturing Engineer (for design transfer and process validation)
- Intellectual Property Attorney (to maintain and expand patent strategy)
- Graphic Designer/Labeling Specialist (to finalize user instructions and packaging compliance)
| Phase | Contributors |
| Concept | Inventor, Mechanical Engineer, Clinical Advisor |
| Prototype | Mechanical Engineer, Prototyping Tech, Industrial Designer |
| Testing & Validation | Mechanical Engineer, QA Specialist, Sterilization Consultant |
| FDA Submission | Regulatory Affairs Expert, QA Specialist |
| Production & Launch | Manufacturing Engineer, Regulatory Expert, Project Manager |
As the team evolves, contributors may overlap roles, for instance, an experienced mechanical engineer may initially cover early DFM and verification documentation. The goal is not staffing volume but functional coverage and readiness for handoff between phases.
Strategic Takeaway
This project demands a lean but highly capable team with mechanical design at its core and specialty support in sterilization, regulatory affairs, and usability. Establishing clear responsibilities early and phasing in specialized contributors at key milestones will reduce inefficiencies, avoid gaps in compliance, and support a smooth transition from concept to launch.
RISK MITIGATION STRATEGIES
While the Surgical Skin Stapler is a Class I device, its mechanical complexity, reusable design, and clinical function introduce real risks that must be proactively addressed. Effective risk mitigation ensures both regulatory compliance and product reliability in surgical environments.
Usability Risks
- Risks
- High trigger force may cause hand fatigue or incomplete staple deployment.
- Poor ergonomics may affect handling for users with varying hand sizes.
- Confusing reloading or cleaning steps could result in improper assembly or unsafe reuse.
- Mitigation Strategies
- Conduct formative usability testing across user profiles (e.g., surgeons, nurses, techs).
- Provide visual and intuitive IFU instructions, ideally with diagrams.
- Design tactile and audible feedback (e.g., a "click") to confirm staple deployment.
Performance Risks
- Risks
- Inconsistent staple depth or misformed staples may lead to poor wound closure.
- Mechanical misfires may delay surgery or cause user frustration.
- Staple jams or misloads (if applicable) could damage tissue or the device.
- Mitigation Strategies
- Test and document acceptable force ranges for staple actuation.
- Conduct accelerated life-cycle testing to simulate repeated use.
- Implement wear indicators or tracking methods for device lifespan.
Mechanical Safety Risks
- Risks
- Spring or latch failure could release components under tension.
- Deformation from repeated sterilization may cause binding or misalignment.
- Mitigation Strategies
- Use high-strength materials for moving parts (e.g., stainless steel or PEEK).
- Add mechanical stops to prevent overtravel or misalignment.
- Simulate 100+ sterilization cycles to evaluate fatigue and wear.
Regulatory Risks
- Risks
- Incomplete cleaning validation could halt market clearance.
- Underestimating documentation needs (design controls, labeling) may lead to audit issues, even without a 510(k).
- Misclassification could delay submission or trigger additional testing.
- Mitigation Strategies
- Follow FDA’s Reusable Devices Guidance for cleaning validation (FDA 2015).
- Begin compiling a full Design History File (DHF) from Phase I.
- Engage a regulatory expert to confirm Class I Exempt eligibility.
Manufacturing & Supply Chain Risks
- Risks
- Variability in off-the-shelf component tolerances may affect function.
- Material substitutions could introduce sterilization incompatibility.
- Difficult mechanical assembly may reduce repeatability and raise labor costs.
- Mitigation Strategies
- Qualify multiple vendors with strict spec controls.
- Develop assembly fixtures or jigs to ensure mechanical alignment.
- Verify post-sterilization mechanical integrity during pilot builds.
Strategic Takeaway
This stapler’s risk profile isn’t defined by electronics, but by precision mechanics, long-term reusability, and performance under sterilization. Treating this Class I device with the same rigor applied to Class II products, especially in documentation, testing, and validation, will position it for long-term success and reduced market-entry friction.INVESTMENT & FINANCIAL OUTLOOK
Bringing a reusable mechanical device like this Surgical Skin Stapler to market involves balancing engineering investment, regulatory readiness, and cost-to-value optimization. Because it avoids electronics and software, early development costs are likely focused on mechanical design and testing. However, its reusability, sterilization validation, and precision engineering still require careful budgeting.
Primary Cost Drivers
Even for a Class I device, a few specific areas will account for the majority of development costs:
- Mechanical Engineering & Prototyping
Precision mechanical systems, especially with multiple moving parts, require iterative CAD work, tolerance tuning, and real-world testing to refine. - Sterilization & Reuse Validation
Reusable device claims must be backed by robust data on cleaning, disinfection, and performance retention over multiple cycles. Simulated-use testing and cleaning studies can be resource-intensive. - Biocompatibility Testing
Despite superficial skin contact, ISO 10993 testing (cytotoxicity, irritation, sensitization) is still required and must be performed on final materials and processes. - Manufacturing Setup
Tooling, assembly processes, and quality control mechanisms must be established to ensure device consistency over production runs.
Budgeting Tips for Early Inventors
- Plan for multiple prototypes
Mechanical refinement often takes more than one build to get right, especially for trigger systems, spring tension, or staple feed paths. - Start regulatory planning early
Even if you’re Class I exempt, a complete Design History File and cleaning validation effort must be factored into time and cost. - Focus on final materials sooner
Since biocompatibility and sterilization testing require finished materials and processes, minimizing material changes post-testing helps avoid costly retesting. - Track costs by development phase
Separating design, prototyping, testing, and transfer-to-manufacturing costs will help when pitching to investors or applying for grants.
Funding Strategy Considerations
This project is well-suited for staged investment models:
- Seed or pre-seed capital can fund early concept modeling, IP strategy expansion, and prototype development.
- Grant funding (e.g., SBIR, NIH, BARDA) may be available due to the device’s focus on wound care, surgical efficiency, or sustainability (via reuse).
- Strategic partnerships with contract manufacturers or hospital networks could also support validation or pilot deployment in exchange for early access or feedback.
A reusable device with a well-defined procedure fit has potential appeal for impact-driven investors focused on reducing surgical waste, supporting global health, or decreasing healthcare procedure costs.
Revenue Potential Considerations
- Direct unit sales
Hospitals and surgical centers may purchase a limited number of reusable staplers with occasional cartridge or maintenance replacements. - Refillable revenue model
If the device includes proprietary staple cartridges, this opens a recurring revenue opportunity. - Bundled packaging
Offering the stapler alongside wound closure kits or sterile packs could increase adoption in procedural use environments.
Price sensitivity will vary by region, but in cost-conscious or sustainability-focused systems, a well-validated reusable stapler may command premium interest if it clearly outperforms disposables over its lifecycle.
Financial Risk Mitigation
- Use lifecycle testing data to establish a compelling cost-per-use comparison vs. disposables.
- Design for manufacturability early to avoid cost creep in tooling or production ramp-up.
- Ensure IP protection is broad enough to avoid copycat designs and safeguard future licensing or distribution negotiations.
Strategic Takeaway
This device’s investment strategy should highlight its low-tech efficiency, long-term cost savings, and eco-conscious reusability. With relatively modest funding, it can progress through early phases and appeal to strategic investors or partners seeking practical surgical tools that are sustainable, safe, and cost-effective.
Your Complimentary Q&A
Have questions about the report?
Book a 15-minute call to clarify insights or prioritize next steps.
Understanding Vendor Tiers and Impact on Project Cost and Time
Tier 1: Higher costs associated with comprehensive services complete system development, advanced technology, and the ability to manage complex projects. Design services may have shorter lead times due to ability to build a larger team however the scale of operations and the complexity of the more comprehensive supply chain may slow certain processes.
Tier 2: Their cost and Time may vary based on their specialization allowing for efficient production of specific components, potentially leading to shorter lead times for those items. However, since they do not provide complete systems, the overall integration into larger assemblies may require additional coordination, potentially affecting timelines.
Tier 3: Lower costs due to specialization in specific components or materials or limited staffing resources requiring additional coordination with other suppliers. This may slow the development time from both a design and supply chain perspective.
Considerations
- Despite higher costs and longer lead times, Tier 1 suppliers may be more suitable for complex projects requiring integrated solutions.
- For projects with budget constraints, engaging multiple Tier 3 suppliers could be more cost-effective, but may require more intensive project management.
- Working with Tier 3 suppliers entails coordinating a robust supply chain to ensure timely delivery and quality assurance.
The choice between Tier 1 and Tier 3 suppliers involves trade-offs between cost, time, and supply chain management complexity. Careful evaluation of project requirements and resources is essential for making an informed decision.
Disclaimers & Limitations
- Generalizations: This report provides a high-level overview based on standard assumptions and does not account for unique device characteristics. Actual costs, timelines, and risks may vary significantly depending on the device's design, use case, and target market.
- Assumptions of Device Class and Use: Assumptions were made regarding the device's classification and intended use. These assumptions can impact regulatory requirements, costs, and timelines. Specific regulatory pathways, for instance, may differ based on the device's risk classification and market entry strategy.
- Market and Regulatory Dynamics: Regulatory requirements and market conditions are subject to change. The report's cost and timeline estimates may be affected by evolving regulatory landscapes, standards, or unforeseen market dynamics, which could delay approval or require additional testing.
- Risk Assessment Limitations: Risk levels and mitigation strategies are based on general device categories and may not fully address specific technical or operational risks unique to the product. Thorough risk assessments should be tailored to the device's complexity, materials, and usage.
- Development Phases and Milestones: The development phases outlined here follow a typical medical device development pathway, but real-world project phases may overlap or require iteration due to unforeseen challenges or design changes.
- Cost and Timeline Variability: The cost and timeline estimates are based on standard industry benchmarks but do not account for project-specific adjustments. Factors like unexpected technical challenges, prototype iterations, or regulatory re-submissions can significantly impact final costs and schedules.
- Reliance on Industry Standards: The report relies on common industry standards for development and testing. However, additional standards specific to certain device features or regions may apply, affecting compliance requirements and associated timelines.
- Testing and Validation Scope: Testing and validation requirements are generalized. Devices with novel materials, complex electronics, or unique features may require additional, specialized tests, potentially extending both cost and duration.
READY FOR EVEN MORE INSIGHTS?
Unlock for $29.95- Regulatory pathway and market opportunity
- Milestone roadmap with phase activities
- Team and resource playbook
- Risk factors and mitigation strategies
- Financial planning and commercialization outlook
UNLOCK NOW
- Development cost and timeline benchmarks
- Complexity insights shaping risk and effort
- Technology readiness snapshot
.png?width=4200&height=441&name=Zewski_Report%20Logo%20(Shirts).png)